Stimulant Use Is Contributing to Rising Fatal Drug Overdoses
Screening, treatment, and strategies to reduce harm can help

Editor's note: This fact sheet was updated on Aug. 23, 2024, to clarify that cocaine and methamphetamine were involved in, rather than accounted for, a percentage of overdose deaths in 2022.
Overview
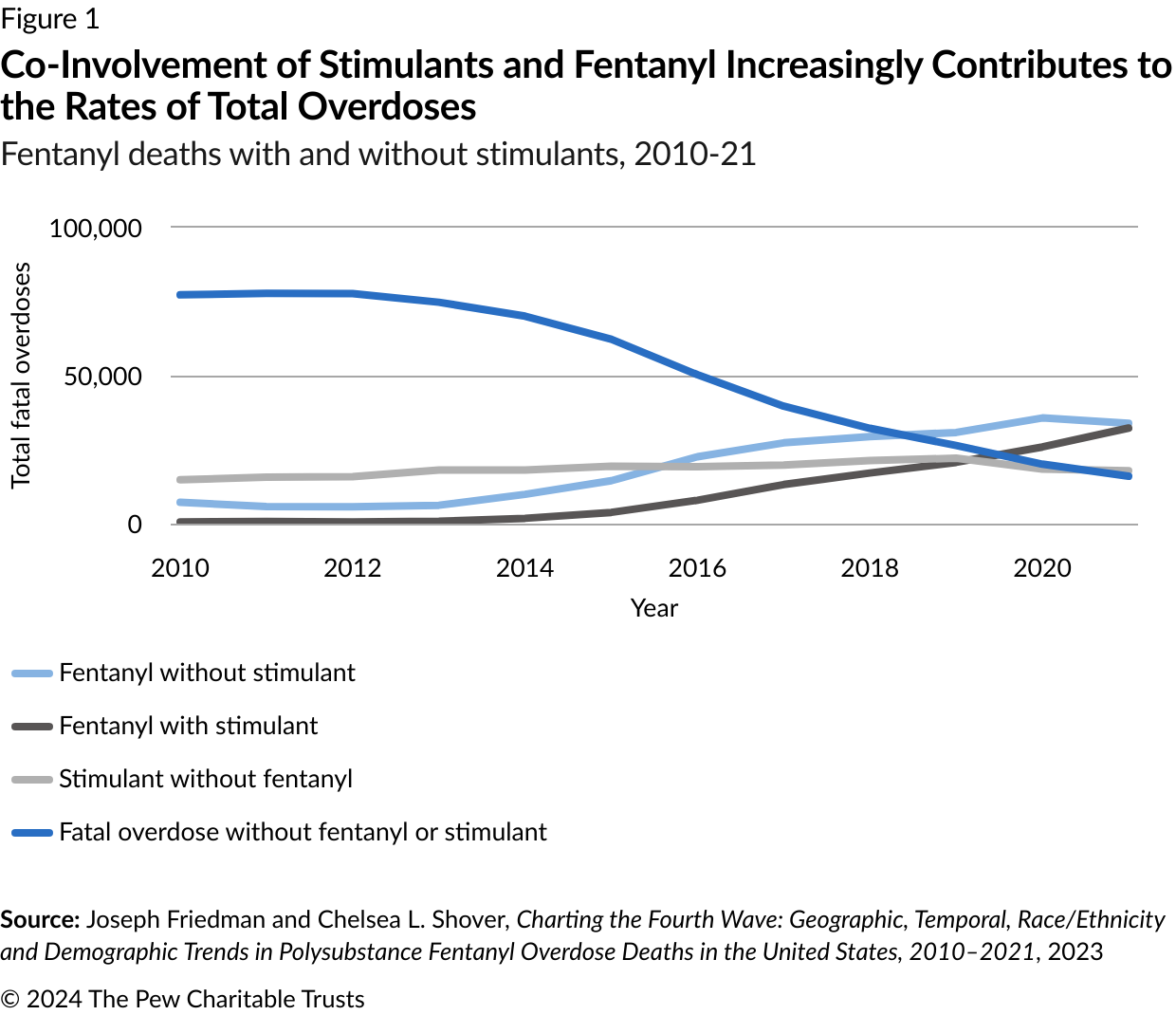
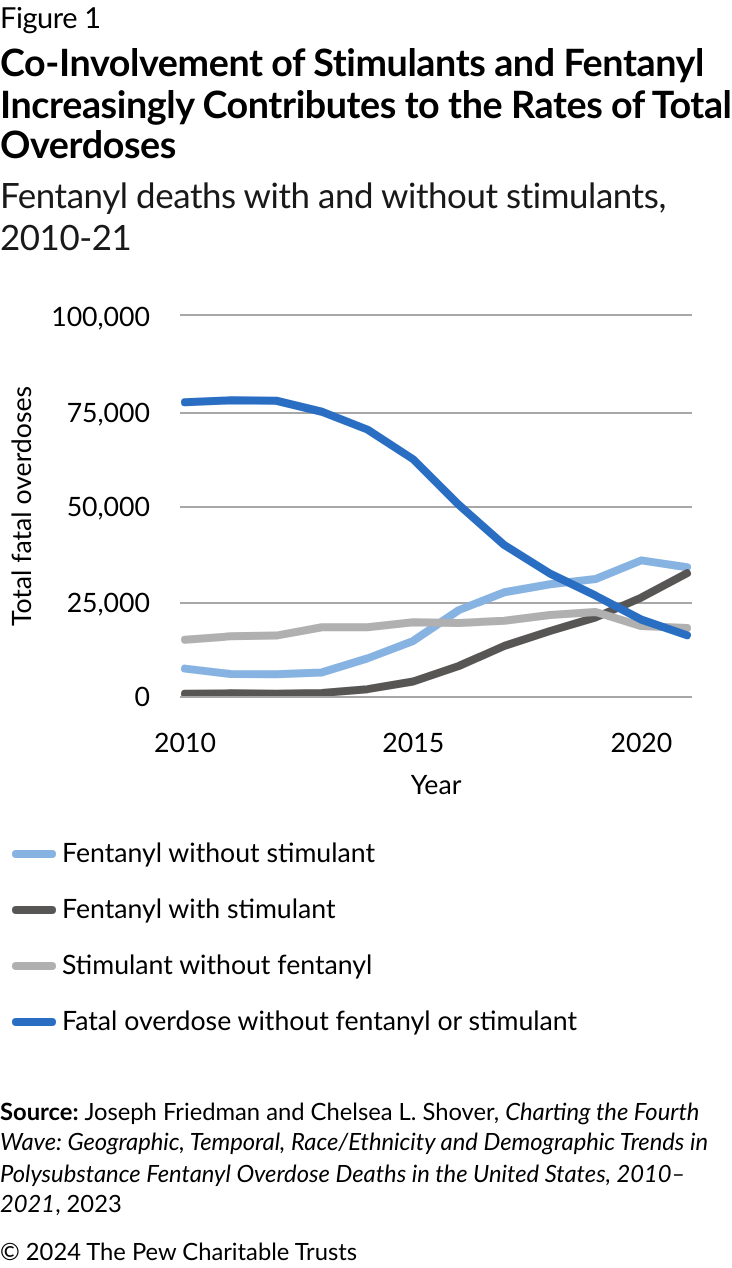
Stimulant use is on the rise across the United States. In 2022, more than 10.2 million people aged 12 and older misused stimulants—a class of drugs that includes cocaine, methamphetamine, and prescription stimulants such as attention-deficit/hyperactivity disorder (ADHD) medications. This is an increase of 8.63% from 2021, when the number was 9.4 million.1 The upward trend has coincided with increasing fentanyl deaths that involve the co-use of stimulants. In 2010, less than 1% of these fatal overdoses involved stimulants—by 2021, that rate had jumped to 32%.2
The use of more than one substance, or polysubstance use, is common among people who use drugs.3 In many cases, combined opioid and stimulant use is intentional, with the user either co-administering the drugs simultaneously or using opioids and stimulants at different times.4 On occasion, the combined use is accidental, with a stimulant contaminated with fentanyl. However they are combined, opioids and stimulants taken together increase overdose risk, especially for people who use stimulants but don’t regularly use opioids.5
What are stimulants?
Stimulants, also referred to as psychostimulants, increase feelings of euphoria, excitement, and alertness. People use stimulants for a variety of reasons: to stay safe and alert while experiencing homelessness; to avoid excessive sedation from opioids; to enhance performance at work or school; to reduce weight; and for pleasure, including to enhance sexual experiences.6 Each stimulant affects the brain differently based on routes of administration and forms of the drug used. Withdrawal following regular use of stimulants can induce intense cravings for the drug, anxiety, agitation, fatigue, increased feelings of depression, and excessive sleepiness.7
Commonly used stimulants include:
Cocaine/crack: Cocaine is a plant-derived stimulant that induces euphoria and is commonly seen in two forms: a powder that can be administered nasally, smoked, injected, or ingested—or a crystallized rock form called “crack” that can be smoked. In 2022, cocaine was involved in 29.7% of overdose deaths within 30 states that report data to the Centers for Disease Control and Prevention.8
Methamphetamine: Methamphetamine also induces euphoria and can exist as a powder or a crystallized solid. These forms of drugs can be administered nasally, smoked, injected, and sometimes inserted rectally. In 2022, methamphetamine was involved in 29.7% of all overdose deaths within 30 states that report data to the CDC.9
Prescription stimulants: Prescription stimulants, like mixed amphetamine salts (Adderall) and methylphenidate (Ritalin), are often used to treat conditions such as attention-deficit/hyperactivity disorder. Prescription stimulants are commonly seen in a pill form and used orally. When misused, the pills can also be crushed and administered nasally.10 Overdose data is limited since deaths from prescription stimulants are often combined with methamphetamine-related overdose deaths under the umbrella term “psychostimulants with abuse potential.”
The most frequently used stimulants vary by region across the country. Methamphetamine is most widely available in the West and Midwest, and while cocaine can be found nationwide, its use is most prevalent in the South and Northeast. However, these patterns change. Recent data shows that methamphetamine is becoming increasingly common in the Northeast, while cocaine use is increasing in select cities in the Midwest and West.11
Stimulant-related deaths are increasing for all racial and ethnic groups, but some communities are affected more than others.12 In 2019, when compared with other racial and ethnic groups, rates of fatal cocaine-involved overdoses were highest in Black populations, and rates of methamphetamine-involved overdoses were highest in American Indian/Alaska Native (AI/AN) populations.13 Other groups with higher rates of stimulant use than the general population include people experiencing homelessness, transgender individuals, and men who have sex with men (MSM).14 In addition, people with mental health issues are also more likely to develop stimulant use disorder (StUD) than people without pre-existing mental health concerns.15
Fortunately, approaches including screening, evidence-based treatment, and lifesaving strategies (also known as harm reduction strategies, such as fentanyl testing strips and syringe service programs) can help reduce the risks of stimulant use and save lives.
Screening for stimulant misuse
Stimulant use often goes undetected in health care settings, such as emergency departments and primary care offices. These are places where people experiencing stimulant overdoses are treated for serious health concerns—such as accidents, cardiovascular concerns, and psychosis (see box below) caused by these drugs. It is uncommon for routine primary care settings to screen for stimulant misuse. 16
The American Society of Addiction Medicine (ASAM) recommends that routine screening for substance use in primary care settings include an assessment for stimulants.17 Although using stimulants as prescribed is not associated with developing a StUD, ASAM also recommends that the best and safest practice is to regularly screen adolescents and adults who are prescribed stimulants for signs of misuse.18
But in primary care and intensive medical settings, screening for stimulant misuse can present challenges for clinicians not familiar with treating people who misuse these drugs. Many clinicians who aren’t familiar with StUD and its treatment don’t follow the recommended protocol of using standardized screening tools or urine drug screens—or even ask about specific drug use; instead, they rely on the patient or relatives to disclose stimulant use. And if patients don’t discuss such use, health providers can miss the links between health conditions for the patient visit that might involve stimulant use/misuse in otherwise healthy individuals.19
In the emergency department, health care providers who use screening initiatives to link patients to medications for opioid use disorder (OUD) have realized they are missing opportunities to connect patients with StUD to care.20 Such interventions can help patients to get care in the community, access treatments to improve health, and return to the emergency department less frequently.21
Screening in health settings can also be beneficial for the many people who use stimulants but do not meet the criteria for a substance use disorder.22 If health providers can identify stimulant use, they can start a conversation with patients about mitigating related health risks and coordinating lifesaving strategies. ASAM recommends that health providers talk to patients who screen positive for stimulant misuse about their frequency and amount of use, route of administration, and other behaviors associated with stimulant misuse.23
The Substance Abuse and Mental Health Services Administration (SAMHSA) recommends that clinicians use destigmatizing language related to gender, sexual orientation, and race and ethnicity when screening patients for stimulant misuse. Such language increases the chance that patients will talk honestly about their stimulant use and ultimately accept being referred or linked to treatment if appropriate.24
What Does a Stimulant Overdose Look Like?
Unlike opioid overdoses, stimulant overdoses are not defined by a single symptom. Instead, they happen when people use a toxic level of a stimulant that produces a range of adverse physical and psychological reactions.25 These events are sometimes referred to as “overamping” to distinguish them from opioid overdoses, which are marked by respiratory depression.26
Common symptoms of stimulant overdoses or overamping include:
| Physical | Psychological | ||
|---|---|---|---|
| Nausea or vomiting High fever, overheating, or excessive sweating Irregular breathing and shortness of breath Dizziness Tremors Chest pain |
Increased heart rate and racing pulse Heart palpitations Convulsions or seizures Severe headache Heart attack and stroke |
Psychosis (mania, delusions, illusions, disorganized thought or speech) Hallucinations Agitation Paranoia |
Extreme anxiety Panic Increased aggressiveness Hypervigilance |
Sources: National Harm Reduction Coalition, “Stimulant Overamping Basics”; SAMHSA, “Treatment for Stimulant Use Disorders” (2021); Centers for Disease Control and Prevention, “A Stimulant Guide”; North Carolina Harm Reduction Coalition, “Speed Overdose (Overamping)”
The appropriate response to a stimulant overdose depends on the symptoms. Using a cool wet washcloth and ensuring the person is hydrated can lower body temperature, which can help with physical symptoms such as fevers, overheating, and sweating. Calming techniques that include a dark environment can help minimize psychological symptoms.
In serious cases, overamping can be fatal.27 So if symptoms worsen, or if a person appears to be suffering from a heart attack, stroke, or seizure, then emergency medical attention is critical. Such serious events can worsen or be caused by previous damage to the cardiovascular system due to chronic stimulant use.28 If the co-use of opioids is a possibility, the person should be administered naloxone.29
Treating stimulant use disorder
In 2022, survey data showed that an estimated 4.5 million people had a StUD, but that only 888,000 received treatment.30
Unlike OUD, there are no medications approved by the U.S. Food and Drug Administration to treat StUD. In 2023, ASAM and the American Academy of Addiction Psychiatry (AAAP) released the Clinical Practice Guideline on the Management of Stimulant Use Disorder, which provides evidence-based treatment options and screening guidelines for clinicians treating those with StUD.31
According to these guidelines, the standard of care is an approach called contingency management (CM).32 In some cases, off-label medications—meaning drugs approved by the FDA for other conditions—can also be used.33
Contingency management
CM is a behavioral therapy that provides a patient with valuable rewards for demonstrated positive behaviors.34 CM is effective on its own to meet patient goals, and also can be used to attract patients to treatment and keep them engaged in care for reducing stimulant use; it’s often used along with other behavioral therapies and medications to treat other disorders, such as opioid use and alcohol use disorders.
Decades of research has found that CM is associated with longer durations of stimulant abstinence during treatment and higher rates of adherence to treatment than other behavioral therapies.35 Recipients of CM are more likely to show abstinence at follow-up than people in other forms of treatment.36 Additionally, it’s the standard of care for addressing stimulant use disorder within the Veterans Health Administration.37 The approach generates a high return on investment: For every $1 invested in CM for drug and alcohol use disorders, more than $30 of societal benefits are gained.38
How Contingency Management Works
- The provider and patient agree on one objectively verifiable target behavior that is both related to stimulant use and can be achievable by the patient.39 Common target behaviors are treatment attendance or stimulant abstinence.40
- The provider monitors whether the agreed-upon behavior occurred, usually through a urine drug test to verify stimulant abstinence.41 This monitoring occurs two to three times a week.42
- If patients demonstrate compliance with the agreed-upon behavior, they are rewarded immediately, often with gift cards greater than $5 or $16.43 Successive demonstrations of compliance with the behavior earn increased awards.44 If patients don’t demonstrate compliance, they do not receive the reward but are encouraged to try again.45
- The treatment should last a minimum of 12 weeks, though longer durations are more effective.46
Although CM is an effective treatment, its elements must be implemented correctly to reach and maintain positive outcomes. Rewards must be high enough to be valuable to the client. While research shows that potential cumulative earning amounts of $400-$560 can be effective at reducing stimulant use, greater reductions of use occur with higher amounts over the course of treatment.47 These rewards must be provided frequently and delivered immediately to the client when they demonstrate the desired positive behavior, such as a urine drug screen that is negative for stimulants.48
However, federal rules that limit funding for incentives, as well as rules that limit total cumulative annual incentive amounts, present barriers for most state officials hoping to implement CM. States offering CM using SAMHSA-funded grant program funds can offer only a maximum of $75 per patient each year, which is far below the evidence-based cumulative incentive amounts.49
Additionally, potential providers of CM services are wary of violating federal laws known as the Anti-Kickback Statute and Civil Monetary Penalties Law. These laws prohibit providers from using incentives to influence referrals and patient choice and are meant to prevent fraud, waste, and abuse of Medicare and Medicaid resources.50
Advocates, including the AAAP, ASAM, and members of Congress, have called for federal policy changes to remove these barriers.51 Specifically, these advocates have asked the Department of Health and Human Services (HHS) Office of Inspector General (which oversees all HHS agencies, including the Centers for Medicare & Medicaid Services and SAMHSA) to issue guidance for implementing CM without violating these laws. Such guidance may prompt SAMHSA to increase the $75 annual limit.52
HHS recently released a report describing barriers to effective CM implementation, demonstrating that HHS officials are aware that current federal laws and policies hinder CM treatment.53
One option for implementing CM with the current rules is through the submission and approval of a Medicaid 1115 demonstration waiver, which allows state Medicaid agencies to implement innovative health programs that may deviate from the usual federal Medicaid requirements.54 These waivers would allow states to provide CM to Medicaid recipients with the assurance that states are not violating fraud and abuse laws.55 As of April 2024, California, Washington, and Montana have received approval for their CM waivers.56 However, preparing, submitting, and receiving approval for a Medicaid waiver is a lengthy process.57
Medications
Although there are no FDA-approved medications to treat StUD, research is ongoing and ASAM recommends a limited set of off-label medications that have shown evidence of efficacy.58 For example, bupropion, which is FDA approved to treat depression, seasonal affective disorder, and for helping people quit smoking, and naltrexone, which is FDA-approved to treat opioid and alcohol use disorder, have been shown in clinical trials to help people reduce their methamphetamine use when used in combination.59 The ASAM guideline also acknowledges that research on the use of medications for people with StUD is limited and that clinicians should prescribe these carefully and closely monitor patients’ symptoms and medication adherence.
These medications are most effective at reducing stimulant use—not in creating stimulant abstinence. This reduction in use is associated with benefits for clients such as reduced cravings, drug-seeking behavior, and severity of depression symptoms while improving overall functioning.60 Because of these benefits, medications can be a good choice for people interested in reducing their use of stimulants. If abstinence is the goal, the likelihood of achieving it can be increased when combining medications with contingency management.61
Lifesaving strategies for stimulant use
A number of strategies can be used to reduce the risk of stimulant-involved overdoses and other health challenges associated with the use of these drugs.
Overdose prevention
Because stimulant and opioid use are often combined, SAMHSA, ASAM, and the CDC recommend providing drug-checking equipment to people who use stimulants. Equipment such as test strips can detect whether fentanyl is present in drugs.62 And although there are no specific antidotes to stimulant overdoses or overamping events, naloxone should be used in cases of a suspected opioid-related overdose, which is indicated by a person not breathing.63
Strategies to reduce harm
Lifesaving strategies, also known as harm reduction, can also reduce the risk and transmission of other health problems associated with stimulant use, including viral and bacterial infections, sexually transmitted infections, and other health conditions. These strategies include:
- Stigma-free health care services that consider the needs of special populations can increase the likelihood of a person seeking medical care, disclosing risky behavior, and agreeing to screening for HIV and hepatitis C (HCV).64
- Access to stable housing and Housing First programs, which don’t require abstinence for people to attain or maintain housing, decreases substance use and related physical harms.65
- Syringe service programs distribute free new sterile needles to people who inject drugs.66 Although often focused on those with OUD, these programs can serve people who inject stimulants, reducing their risk of HIV and HCV. These programs can also expand to include those who administer drugs nasally or smoke them by providing these people with supplies to reduce physical harms related to these routes of administration, such as infections caused by sharing equipment.67
- Safer sex supplies and the medication known as pre-exposure prophylaxis (PrEP) can reduce the risk of HIV transmission, which is elevated among people who inject stimulants and certain populations of people who prefer to use stimulants when engaging in sexual behavior.68
Conclusion
Stimulant use and fatal overdoses related to stimulant use are increasing.69 Expanded access to evidence-based strategies such as screening, effective treatment, and lifesaving strategies that reduce harm is necessary to save lives and improve the health and well-being of people who use stimulants.
Endnotes
- Center for Behavioral Health Statistics and Quality, “Results From the 2022 National Survey on Drug Use and Health: Detailed Tables,” Substance Abuse and Mental Health Services Administration, 2023, https://www.samhsa.gov/data/report/2022-nsduh-detailed-tables.
- Joseph Friedman and Chelsea L. Shover, “Charting the Fourth Wave: Geographic, Temporal, Race/Ethnicity and Demographic Trends in Polysubstance Fentanyl Overdose Deaths in the United States, 2010–2021,” Addiction 118, no. 12 (2023): 2477-85, https://doi.org/10.1111/ add.16318.
- Elizabeth A. Crummy et al., “One Is Not Enough: Understanding and Modeling Polysubstance Use,” Frontiers in Neuroscience 14 (2020): https://www.frontiersin.org/articles/10.3389/fnins.2020.00569.
- A. Al-Tayyib et al., “Heroin and Methamphetamine Injection: An Emerging Drug Use Pattern,” Substance Use & Misuse 52, no. 8 (2017): 1051-58, https://doi.org/10.1080/10826084.2016.1271432. J. Ondocsin et al., “The Motives and Methods of Methamphetamine and ‘Heroin’ Co-Use in West Virginia,” Harm Reduction Journal 20, no. 1 (2023): 88, https://doi.org/10.1186/s12954-023-00816-8.
- Karla D. Wagner et al., “Prevalence of Fentanyl in Methamphetamine and Cocaine Samples Collected by Community-Based Drug Checking Services,” Drug and Alcohol Dependence 252 (2023): 110985, https://www.sciencedirect.com/science/article/pii/S0376871623012231.
- Stephen V. Faraone et al., “Systematic Review: Nonmedical Use of Prescription Stimulants: Risk Factors, Outcomes, and Risk Reduction Strategies,” Journal of the American Academy of Child & Adolescent Psychiatry 59, no. 1 (2020): 100-12, https://www.sciencedirect.com/science/article/pii/S0890856719304708. Callan Elswick Fockele et al., “‘That Line Just Kept Moving’: Motivations and Experiences of People Who Use Methamphetamine,” Western Journal of Emergency Medicine 24, no. 2 (2023): 218-27, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10047723/. Rebecca L. Haffajee and Sara Heins, “State and Community Efforts to Address Stimulant Use,” RAND Corporation, 2021, https://aspe.hhs.gov/reports/state-community-efforts-address-stimulant-use. Christopher M. Jones et al., “Methamphetamine Use in the United States: Epidemiological Update and Implications for Prevention, Treatment, and Harm Reduction,” Annals of the New York Academy of Sciences 1508, no. 1 (2022): 3-22, https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC9097961/.
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders,” 2021, https://store.samhsa.gov/sites/default/files/pep21-02-01-004.pdf.
- “State Unintentional Drug Overdose Reporting System (SUDORS),” Centers for Disease Control and Prevention, Jan. 17, 2023, https://www.cdc.gov/overdose-prevention/data-research/facts-stats/sudors-dashboard-fatal-overdose-data.html.
- “State Unintentional Drug Overdose Reporting System (SUDORS),” Centers for Disease Control and Prevention.
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.”
- U.S. Drug Enforcement Administration, “The 2019 National Drug Threat Assessment (NDTA),” 2019, https://www.dea.gov/sites/default/files/2020-01/2019-NDTA-final-01-14-2020_Low_Web-DIR-007-20_2019.pdf.
- Center for Behavioral Health Statistics and Quality, “2022 National Survey on Drug Use and Health: Detailed Tables.” National Institute for Health Care Management Foundation, “Stimulant Death Rates Climbed Across Races and Ethnicity,” 2022.
- Mbabazi Kariisa et al., “Drug Overdose Deaths Involving Cocaine and Psychostimulants With Abuse Potential Among Racial and Ethnic Groups—United States,” 2004–2019,” Drug and Alcohol Dependence 227 (2021): 109001, https://www.sciencedirect.com/science/article/pii/S0376871621004968.
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.”
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.”
- Julia Dunn et al., “Addressing Methamphetamine Use in Primary Care: Provider Perspectives,” Journal of Addiction Medicine 17, no. 1 (2023): https://journals.lww.com/journaladdictionmedicine/fulltext/2023/01000/addressing_methamphetamine_use_in_primary_ care_.16.aspx. Leslie W. Suen et al., “Emergency Department Visits and Trends Related to Cocaine, Psychostimulants, and Opioids in the United States, 2008–2018,” BMC Emergency Medicine 22, no. 1 (2022): 19, https://doi.org/10.1186/s12873-022-00573-0.
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline on the Management of Stimulant Use Disorder,” 2023, https://www.asam.org/quality-care/clinical-guidelines/stimulant-use-disorders.
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- Julia Dunn et al., “Addressing Methamphetamine Use.”
- Cindy Parks Thomas et al., “Emergency Department Interventions for Opioid Use Disorder: Overview of the Landscape, Key Components, and Analysis of Five Case Studies,” 2023, https://aspe.hhs.gov/sites/default/files/documents/4da0bd61a6c21dafaf58459b1de79718/ed-interventions-oud.pdf.
- Scott A. Simpson et al., “Evaluation of the BEAT Meth Intervention for Emergency Department Patients With Methamphetamine Psychosis,” Journal of Addiction Medicine 17, no. 1 (2023): 67-73, https://journals.lww.com/journaladdictionmedicine/fulltext/2023/01000/evaluation_of_the_beat_meth_intervention_for.18.aspx.
- Joshua C. Black et al., “Initiation Patterns and Transitions Among Adults Using Stimulant Drugs: Latent Transition Analysis,” Journal of Medical Internet Research 25 (2023): e46747, https://www.jmir.org/2023/1/e46747.
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.”
- J.J. Carroll, T.C. Green, and S. Mital, “Stimulant Guide” (Centers for Disease Control and Prevention, 2022), https://www.cdc.gov/drugoverdose/featured-topics/stimulant-guide.html.
- National Harm Reduction Coalition, ”Stimulant Overamping Basics,” accessed Aug. 31, 2020, https://harmreduction.org/issues/overdose-prevention/overview/stimulant-overamping-basics/what-is-overamping/.
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.”
- Elise D. Riley, Priscilla Y. Hsue, and Phillip O. Coffin, “A Chronic Condition Disguised as an Acute Event: The Case for Re-Thinking Stimulant Overdose Death,” Journal of General Internal Medicine 37, no. 13 (2022): 3462-64, https://doi.org/10.1007/s11606-022-07692-1.
- “Speed Overdose (Overamping),” North Carolina Harm Reduction Coalition, Jan. 23, 2024, https://www.nchrc.org/naloxone-odprevention-2/speed-overdose-overamping/. Jennifer J. Carroll, Traci C. Green, and Sasha Mital, “Stimulant Guide.”
- Center for Behavioral Health Statistics and Quality, “2022 National Survey on Drug Use and Health: Detailed Tables.”
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- P.V. AshaRani et al., “Non-Pharmacological Interventions for Methamphetamine Use Disorder: A Systematic Review,” Drug and Alcohol Dependence 212 (2020): 108060, https://www.sciencedirect.com/science/article/pii/S0376871620302258.
- Meredith K. Ginley et al., “Long-Term Efficacy of Contingency Management Treatment Based on Objective Indicators of Abstinence From Illicit Substance Use Up to 1 Year Following Treatment: A Meta-Analysis,” Journal of Consulting and Clinical Psychology 89, no. 1 (2021): 58-71, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8034391/pdf/nihms-1687070.pdf.
- Dominick DePhilippis et al., “History and Current Status of Contingency Management Programs in the Department of Veterans Affairs,” Preventive Medicine 176 (2023): 107704, https://www.sciencedirect.com/science/article/pii/S0091743523002840.
- Washington State Institute for Public Policy. “Contingency Management (Higher Cost) for Substance Use Disorders,” https://www.wsipp.wa.gov/BenefitCost/Program/297.
- Lynn McIntosh, “Contingency Management Part 2: The Founding Principles,” Northwest Frontier Addiction Technology Transfer Center, accessed March 18, 2024, https://attcnetwork.org/contingency-management-part-2-the-founding-principles/.
- Lynn McIntosh, “Contingency Management Part 2: The Founding Principles.”
- Lynn McIntosh, “Contingency Management Part 2: The Founding Principles.”
- Carla J. Rash, “Implementing an Evidence-Based Prize Contingency Management Protocol for Stimulant Use,” Journal of Substance Use and Addiction Treatment 151 (2023): 209079, https://www.sciencedirect.com/science/article/pii/S2949875923001303. John M. Roll and Steve Shoptaw, “Contingency Management: Schedule Effects,” Psychiatry Research 144, no. 1 (2006): 91-93, https://www.sciencedirect.com/science/article/pii/S0165178105003884.
- Carla J. Rash, “Implementing an Evidence-Based Prize Contingency Management Protocol for Stimulant Use.” John M. Roll and Steve Shoptaw, “Contingency Management: Schedule Effects.”
- Carla J. Rash, “Implementing an Evidence-Based Prize Contingency Management Protocol for Stimulant Use.” John M. Roll and Steve Shoptaw, “Contingency Management: Schedule Effects.”
- John M. Roll and Steve Shoptaw, “Contingency Management: Schedule Effects.”
- John M. Roll et al., “Duration Effects in Contingency Management Treatment of Methamphetamine Disorders,” Addictive Behaviors 38, no. 9 (2013): 2455-62, https://pubmed.ncbi.nlm.nih.gov/23708468/. Substance Abuse and Mental Health Services Administration, “Treatment of Stimulant Use Disorders,” 2020, https://store.samhsa.gov/product/treatment-stimulant-use-disorders/pep20-06-01-001.
- Carla J. Rash and Dominick DePhilippis, “Considerations for Implementing Contingency Management in Substance Abuse Treatment Clinics: The Veterans Affairs Initiative as a Model,” Perspectives on Behavior Science 42, no. 3 (2019): 479-99, https://doi.org/10.1007/s40614-019-00204-3.
- Carla J. Rash, Sheila M. Alessi, and Kristyn Zajac, “Examining Implementation of Contingency Management in Real-World Settings,” Psychology of Addictive Behaviors 34, no. 1 (2020): 89, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6980876/. Richard A. Rawson et al., “Contingency Management for Stimulant Use Disorder: Progress, Challenges, and Recommendations,” Journal of Ambulatory Care Management 46, no. 2 (2023): 152-59, https://journals.lww.com/ambulatorycaremanagement/abstract/2023/04000/contingency_management_for_stimulant_use_disorder_.14.aspx.
- Substance Abuse and Mental Health Services Administration, “FY 2024 Substance Abuse and Mental Health Services Administration (SAMHSA) Notice of Funding Opportunity (NOFO) Application Guide,” 2024, https://www.samhsa.gov/sites/default/files/fy-2024-grant-application-guide.pdf. Michael G. McDonell et al., “Federal Policy Changes Must Occur to Provide a Lifesaving Stimulant Drug Intervention,” Health Affairs Forefront, Feb. 14, 2024, https://www.healthaffairs.org/content/forefront/federal-policy-changes-must-occur-provide-lifesaving-stimulant-drug-intervention.
- U.S. Department of Health and Human Services, “Contingency Management for the Treatment of Substance Use Disorders: Enhancing Access, Quality, and Program Integrity for an Evidence-Based Intervention,” 2023, https://aspe.hhs.gov/sites/default/files/documents/72bda5309911c29cd1ba3202c9ee0e03/contingency-management-sub-treatment.pdf.
- American Academy of Addiction Psychiatry et al., Re: Oig-128-N, Solicitation of New Safe Harbors and Special Fraud Alerts to Christi A. Grimm, principal deputy inspector general at the Office of the Inspector General, https://www.aaap.org/wp-content/uploads/2021/02/AKS-Safe-Harbor-for-CM-Sign-On-Letter.pdf. Richard A. Rawson et al., “Contingency Management for Stimulant Use Disorder: Progress, Challenges, and Recommendations.” Peter Welch et al., members of Congress, Bipartisan Letter to Clarify Treatment Protocols for Stimulant Use Disorder to Xavier Becerra and Dr. Rahul Gupta, secretary, U.S. Department of Health and Human Services, and director, Office of National Drug Control Policy, Dec. 12, 2023, https://www.welch.senate.gov/wp-content/uploads/2023/12/CM-Letter-Final-20231214.pdf.
- Richard A. Rawson et al., “Contingency Management for Stimulant Use Disorder: Progress, Challenges, and Recommendations.”
- U.S. Department of Health and Human Services, “Contingency Management for the Treatment of Substance Use Disorders: Enhancing Access, Quality, and Program Integrity for an Evidence-Based Intervention.”
- Centers for Medicare & Medicaid Services, “About Section 1115 Demonstrations,” accessed April 22, 2024, https://www.medicaid.gov/medicaid/section-1115-demonstrations/about-section-1115-demonstrations/index.html.
- Michael G McDonell et al., “Federal Policy Changes Must Occur.”
- Michael G McDonell et al., “Federal Policy Changes Must Occur.” Kinda Serafi, Virginia E. Morgan, and Benjamin Ahmad, “CMS Approves Montana’s Reentry Services, Contingency Management, and Tenancy Supports 1115 Waiver,” news release, March 6, 2024, https://www.manatt.com/insights/newsletters/health-highlights/cms-approves-montanas-reentry-services-contingen.
- Michael G McDonell et al., “Federal Policy Changes Must Occur.”
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.”
- Masoumeh Amin-Esmaeili et al., “Reduced Drug Use as an Alternative Valid Outcome in Individuals With Stimulant Use Disorders: Findings From 13 Multisite Randomized Clinical Trials,” Addiction 119, no. 5 (2024): 833-43, https://pubmed.ncbi.nlm.nih.gov/38197836/.
- Vítor Soares Tardelli et al., “Contingency Management With Pharmacologic Treatment for Stimulant Use Disorders: A Review,” Behaviour Research and Therapy 111 (2018): 57-63, https://www.sciencedirect.com/science/article/pii/S0005796718301566.
- American Society of Addiction Medicine (ASAM) and American Academy of Addiction Psychiatry (AAAP), “Clinical Practice Guideline.” Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.” Jennifer J. Carroll, Traci C. Green, and Sasha Mital, “Stimulant Guide.”
- Jennifer J. Carroll, Traci C. Green, and Sasha Mital, “Stimulant Guide.”
- Substance Abuse and Mental Health Services Administration, “Treatment for Stimulant Use Disorders.”
- Rafaela Rigoni, Joost Breeksema, and Sara Woods, “Speed Limits: Harm Reduction for People Who Use Stimulants,” Mainline, 2018, https://cdn.sanity.io/files/6u5teakk/production/aef23a7e5203ad136467c1a2b06acef8da650481.pdf?dl=.
- The Pew Charitable Trusts, “Syringe Distribution Programs Can Improve Public Health During the Opioid Overdose Crisis,” 2021, https://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2021/03/syringe-distribution-programs-can-improve-public-health-during-the-opioid-overdose-crisis.
- National Alliance of State and Territorial AIDS Directors, “Stimulant Safety: Getting Amped Up to Reduce Harms When Using Stimulants,” https://nastad.org/resources/stimulant-safety-getting-amped-reduce-harms-when-using-stimulants. Samyukta Singh, Caleb Banta-Green, and Susan Kingston, “Distribution of Safer Drug Smoking Supplies as a Public Health Strategy,” Addictions, Drug & Alcohol Institute, University of Washington, 2022, https://adai.uw.edu/wordpress/wp-content/uploads/SaferSmokingBrief_2022.pdf.
- Katie B. Biello et al., “The Past, Present, and Future of PrEP Implementation Among People Who Use Drugs,” Current HIV/AIDS Reports 18, no. 4 (2021): 328-38, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8286349/. National Alliance of State and Territorial AIDS Directors, “Stimulant Safety: Getting Amped Up to Reduce Harms When Using Stimulants.”
- Mbabazi Kariisa et al., “Drug Overdose Deaths.”