America’s Most Common Drug Problem? Unhealthy Alcohol Use
Few patients know about evidence-based treatment—or have or seek access to it

Overview
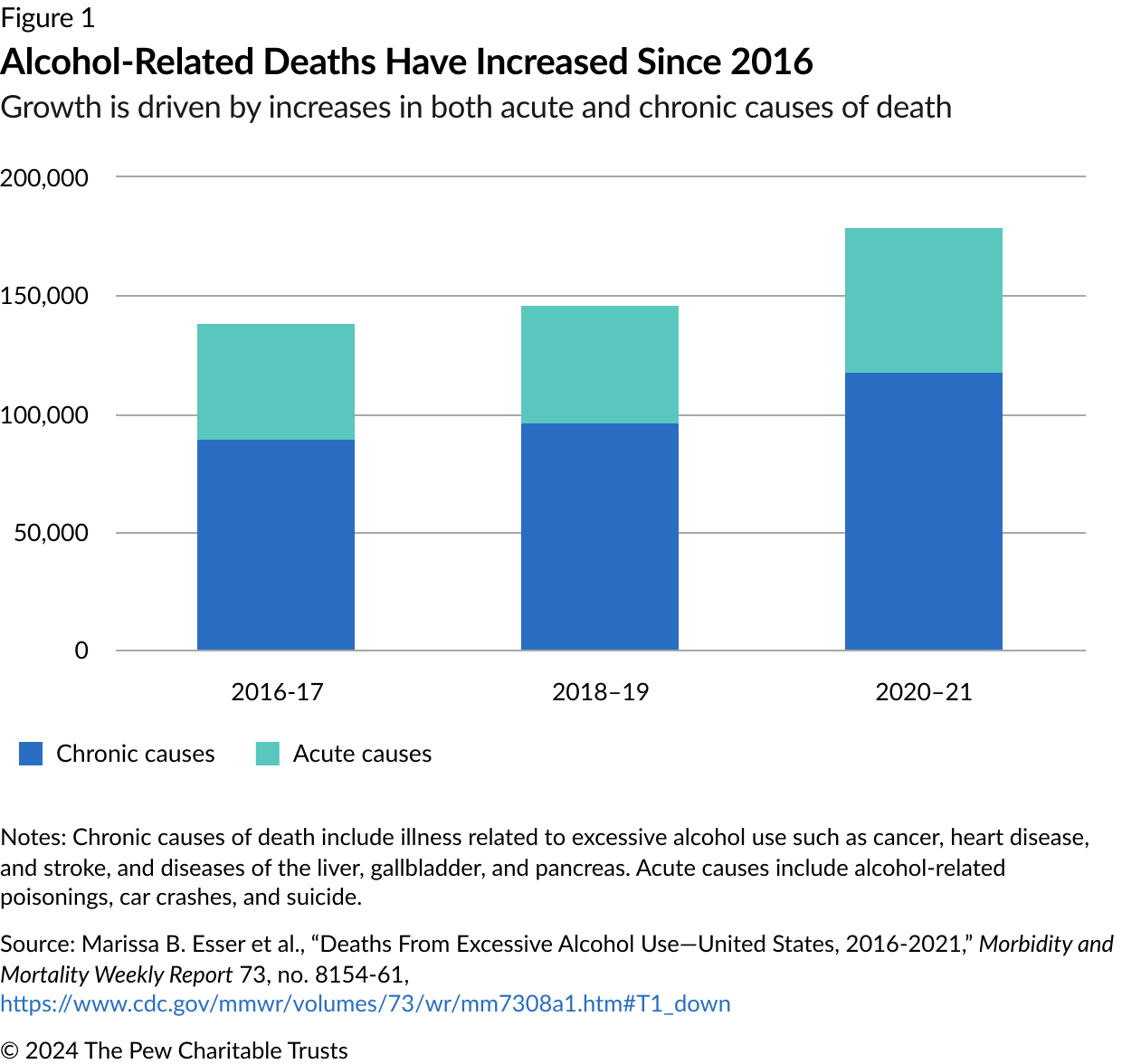
Alcohol is the leading driver of substance use-related fatalities in America: Each year, frequent or excessive drinking causes approximately 178,000 deaths.1 Excessive alcohol use is common in the United States among people who drink: In 2022, of the 137 million Americans who reported drinking in the last 30 days, 45% reported binge drinking (five or more drinks in a sitting for men; four for women).2 Such excessive drinking is associated with health problems such as injuries, alcohol poisoning, cardiovascular conditions, mental health problems, and certain cancers.3
In 2020, many people increased their drinking because of COVID-19-related stressors, including social isolation, which led to a 26% increase in alcohol-related deaths during the first year of the pandemic.4

Nationwide, nearly 30 million people are estimated to have alcohol use disorder (AUD); it is the most common substance use disorder. AUD is a treatable, chronic health condition characterized by a person’s inability to reduce or quit drinking despite negative social, professional, or health effects.5 While no single cause is responsible for developing AUD, a mix of biological, psychological, and environmental factors can increase an individual’s risk, including a family history of the disorder.6
There are well-established guidelines for AUD screening and treatment, including questions that can be asked by a person’s health care team, medications approved by the U.S. Food and Drug Administration (FDA), behavioral therapies, and recovery supports, but these approaches often are not put into practice.7 When policies encourage the adoption of screening and evidence-based medicines for AUD, particularly in primary care, the burden of alcohol-related health problems can be reduced across the country.8
The Spectrum of Unhealthy Alcohol Use
For adults of legal drinking age, U.S. dietary guidelines recommend that they choose not to drink or drink in moderation, defined as two drinks or fewer in a day for men, and one drink or fewer in a day for women.9 One drink is defined as 0.6 ounces of pure alcohol—the amount in a 12-ounce beer containing 5% alcohol, a 5-ounce glass of wine containing 12% alcohol, or 1.5 ounces of 80-proof liquor.10
Consumption patterns exceeding these recommended levels are considered:
- Heavy drinking, defined by the number of drinks consumed per week: 15 or more for men, and eight or more for women.11
- Binge drinking, defined by the number of drinks consumed in a single sitting: five or more for men, and four or more for women.12
Alcohol use disorder is defined by The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as having symptoms of two or more diagnostic criteria within a 12-month period.13 The diagnostic criteria assess behaviors such as trying to stop drinking but being unable to, alcohol cravings, and the extent to which drinking interferes with an individual’s life.14 AUD can be mild (meeting two or three criteria), moderate (meeting four or five criteria), or severe (six or more criteria).15
Identifying and preventing AUD
Primary care providers are well positioned to recognize the signs of unsafe drinking in their patients. The U.S. Preventive Services Task Force recommends that these providers screen adults 18 years and older for alcohol misuse.16 One commonly used evidence-based approach, SBIRT—or screening, brief intervention, and referral to treatment—is a series of steps that help providers identify and address a patient’s problematic substance use.17
Using a screening questionnaire, a provider can determine whether a patient is at risk and, if so, can deliver periodic brief behavioral interventions in an office setting. Such interventions have been shown to reduce heavy alcohol use among adolescents, adults, and older adults.18 When a patient meets the criteria for AUD, providers can offer medication, connect them to specialty treatment, refer them to recovery supports such as Alcoholics Anonymous or other mutual-help groups, or all of the above, depending on a patient’s needs and preferences.19 When these interventions are used in primary care settings, they can reduce heavy alcohol use.20
While screening for AUD is common, few providers follow up when a patient reports problematic alcohol use. From 2015 to 2019, 70% of people with AUD were asked about their alcohol use in health care settings, but just 12% of them received information or advice about reducing their alcohol use.21 Only 5% were referred to treatment.22
Emergency departments (EDs) are another important setting for identifying AUD, and to maintain accreditation they are required to screen at least 80% of all patients for alcohol use.23 Alcohol is the most common cause of substance-related ED visits, meaning many people in these settings are engaged in excessive or risky alcohol consumption and could be linked to care.24
The use of SBIRT in the ED can also reduce alcohol use, especially for people without severe alcohol problems.25 Providers who use SBIRT can help patients reduce future ED visits and also some negative consequences associated with alcohol use, such as injuries.26
Commonly cited barriers to using SBIRT in these health care settings include competing priorities and insufficient treatment capacity in the community when patients need referrals. Conversely, SBIRT use increases with strong leadership and provider buy-in, collaboration across departments and treatment settings, and sufficient privacy to discuss substance use with patients.27
Jails and prisons should also screen for AUD, as well as other SUDs, to assess clinical needs and connect individuals with care. However, screening practices may not be evidence based. A review of the intake forms used to screen individuals in a sample of jails in 2018-19 found that some did not ask about SUD at all, and of those that did, they did not use validated tools accepted for use in health care and SUD treatment settings.28
Withdrawal management
Up to half of all people with AUD experience some withdrawal symptoms when attempting to stop drinking.29 For many, common symptoms such as anxiety, sweating, and insomnia are mild.30 For a small percentage, however, withdrawal can be fatal if not managed appropriately.31 These individuals can experience seizures or a condition called alcohol withdrawal delirium (also referred to as delirium tremens), which causes patients to be confused and experience heart problems and other symptoms; if untreated, it can be fatal.32 People with moderate withdrawal symptoms can also require medical management to address symptoms such as tremors in addition to anxiety, sweating, and insomnia.33
To determine whether a patient with AUD is at risk of severe withdrawal or would benefit from help managing symptoms, the American Society of Addiction Medicine recommends that providers evaluate patients with positive AUD screens for their level of withdrawal risk.34 Based on this evaluation, providers can offer or connect patients to the appropriate level of withdrawal management.35
At a minimum, high-quality withdrawal management includes clinical monitoring and medications to address symptoms.36 Providers may also offer behavioral therapies.37 Depending on the severity of a patient’s symptoms and the presence of co-occurring conditions such as severe cardiovascular or liver disease that require a higher level of care, withdrawal management can be provided on either an inpatient or an outpatient basis.38
According to the U.S. Department of Justice’s Bureau of Justice Assistance and the National Institute of Corrections, jails should also use evidence-based standards of care to address alcohol withdrawal. These standards include screening and assessing individuals who are at risk for withdrawal and, if the jail cannot provide appropriate care, transferring them to an ED or hospital.39
Withdrawal management on its own is not effective in treating AUD, and without additional services after discharge, most people will return to alcohol use.40 Because of this, providers should also connect people with follow-up care, such as residential or outpatient treatment, after withdrawal management to improve outcomes. Continued care helps patients sustain abstinence, reduces their risk of arrests and homelessness, and improves employment outcomes.41
Patients face multiple barriers to this follow-up care, however. For example, withdrawal management providers from the Veterans Health Administration cited long wait times for follow-up care, inadequate housing, and lack of integration between withdrawal management and outpatient services as reasons patients couldn’t access services.42 Patients have also cited barriers such as failure of the withdrawal management provider to arrange continued care, lengths of stay that were too short to allow for recovery to begin, insufficient residential treatment capacity for continued care, and inadequate housing.43
Promising practices for improving care continuity include: providing peer recovery coaches—people with lived expertise of substance use disorder who can help patients navigate treatment and recovery; psychosocial services that increase the motivation to continue treatment; initiating medication treatment before discharge; reminder phone calls; and “warm handoffs,” in which patients are physically accompanied from withdrawal management to the next level of care.44
Treating AUD
In 2023, 29 million people in the U.S. met the criteria for AUD, but less than 1 in 10 received any form of treatment.45 Formal treatment may not be necessary for people with milder AUD and strong support systems.46 But people who do seek out care can face a range of barriers, including stigma, lack of knowledge about what treatment looks like and where to get it, cost, lack of access, long wait times, and care that doesn’t meet their cultural needs.47
For those who need it, AUD treatment can include a combination of behavioral, pharmacological, and social supports designed to help patients reach their recovery goals, which can range from abstaining from alcohol to reducing consumption.48
While for many the goal of treatment is to stop using alcohol entirely, supporting non-abstinence treatment goals is also important, because reduced alcohol consumption is associated with important health benefits such as lower blood pressure, improved liver functioning, and better mental health.49
Services for treating AUD—including medication and behavioral therapy—can be offered across the continuum of care, from primary care to intensive inpatient treatment, depending on a patient’s individual needs.50
Medications
Medications for AUD help patients reduce or cease alcohol consumption based on their individual treatment goals and can help improve health outcomes.51 Medications can be particularly helpful for people experiencing cravings or a return to drinking, or people for whom behavioral therapy alone has not been successful.52 But medications are not often used: Of the 30 million people with AUD in 2022, approximately 2% (or 634,000 people) were treated with medication.53
The FDA has approved three medications to treat AUD:
- Naltrexone reduces cravings in people with AUD.54 This medication is also approved to treat opioid use disorder, and because it blocks the effects of opioids and can cause opioid withdrawal, patients who use these substances must be abstinent from opioids for one to two weeks prior to starting this treatment for AUD.55 It can be taken daily or as needed in a pill or as a monthly injection.56 Oral naltrexone is effective at reducing the percentage of days spent drinking, the percentage of days spent drinking heavily, and a return to any drinking.57 Injectable naltrexone can reduce the number of days spent drinking and the number of heavy drinking days.58 Additionally, naltrexone can reduce the incidence of alcohol-associated liver disease—an often-fatal complication of heavy alcohol use—and slow the disease’s progression in people who already have it.59
- Acamprosate is taken as a pill.60 It reduces alcohol craving and helps people with AUD abstain from drinking.61 It reduces the likelihood of a return to any drinking and number of drinking days.62
- Disulfiram deters alcohol use by inducing nausea and vomiting and other negative symptoms if a person drinks while using it.63 It is also taken as a pill.64 There is insufficient data to determine whether a treatment is more effective than a placebo at preventing relapses in alcohol consumption or other related issues.65 However, for some individuals, knowing they will get sick from consuming alcohol while taking disulfiram can increase motivation to abstain.66 As medication adherence is a challenge for patients, supervised administration of disulfiram by another person—for example, a spouse—can improve outcomes in patients who are compliant.67
Additionally, some medications used “off-label” (meaning they were approved for treating other conditions) have also effectively addressed AUD. A systematic review found that topiramate, a medication approved for treating epilepsy and migraines, had the strongest evidence among off-label drugs for reducing both any drinking and heavy drinking days.68 Like naltrexone, it can reduce the incidence of alcohol-related liver disease.69
Despite the benefits that medications provide, they remain an underutilized tool for a variety of reasons—such as lack of knowledge among patients and providers, stigma against the use of medication, and failure of pharmacies to stock the drugs.70
Behavioral therapies
Behavioral therapies can also help individuals manage AUD, and they support medication adherence:
- Motivational enhancement therapy focuses on steering people through the stages of change71 by reinforcing their motivation to modify personal drinking behaviors.72
- Cognitive behavioral therapy addresses people’s feelings about themselves and their relationships with others and helps to identify and change negative thought patterns and behaviors related to drinking, including recognizing internal and external triggers. It focuses on developing and practicing coping strategies to manage these triggers and prevent continued alcohol use.73
- Contingency management uses positive reinforcement to motivate abstinence or other healthy behavioral changes.74 It can help people who drink heavily to reduce their alcohol use.75
All of these approaches can help address AUD, and no one treatment has proved more effective than another in treating this complicated condition.76 Combining behavioral therapies with other approaches such as medication and recovery supports, as described below, can improve their efficacy.77
Recovery supports
Peer support specialists and mutual-help groups can also help people achieve their personal recovery goals:
- Peer support specialists are individuals with lived expertise in recovery from a substance use disorder who provide a variety of nonclinical services, including emotional support and referrals to community resources.78 The inclusion of peer support specialists in AUD treatment programs has been found to significantly reduce alcohol use and increase attendance in outpatient care.79
- Mutual-help groups, such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART), support individuals dealing with a shared problem. People may seek out these groups more than behavioral or medication treatment for AUD because they can join on their own time and at no cost, and they may better cater to people’s needs related to varying gender identities, ages, or races.80 Observational research shows that voluntary attendance at peer-led AA groups can be as effective as behavioral treatments in reducing drinking.81
People with AUD can use recovery supports on their own, in combination with behavioral treatment or medication, or as a method to maintain recovery when leaving residential treatment or withdrawal management.82
Disparities in alcohol-related deaths and treatment access
While the U.S. records more than 178,000 alcohol-related deaths each year, some populations have a higher risk of alcohol-related deaths, and others face greater barriers to treatment.83
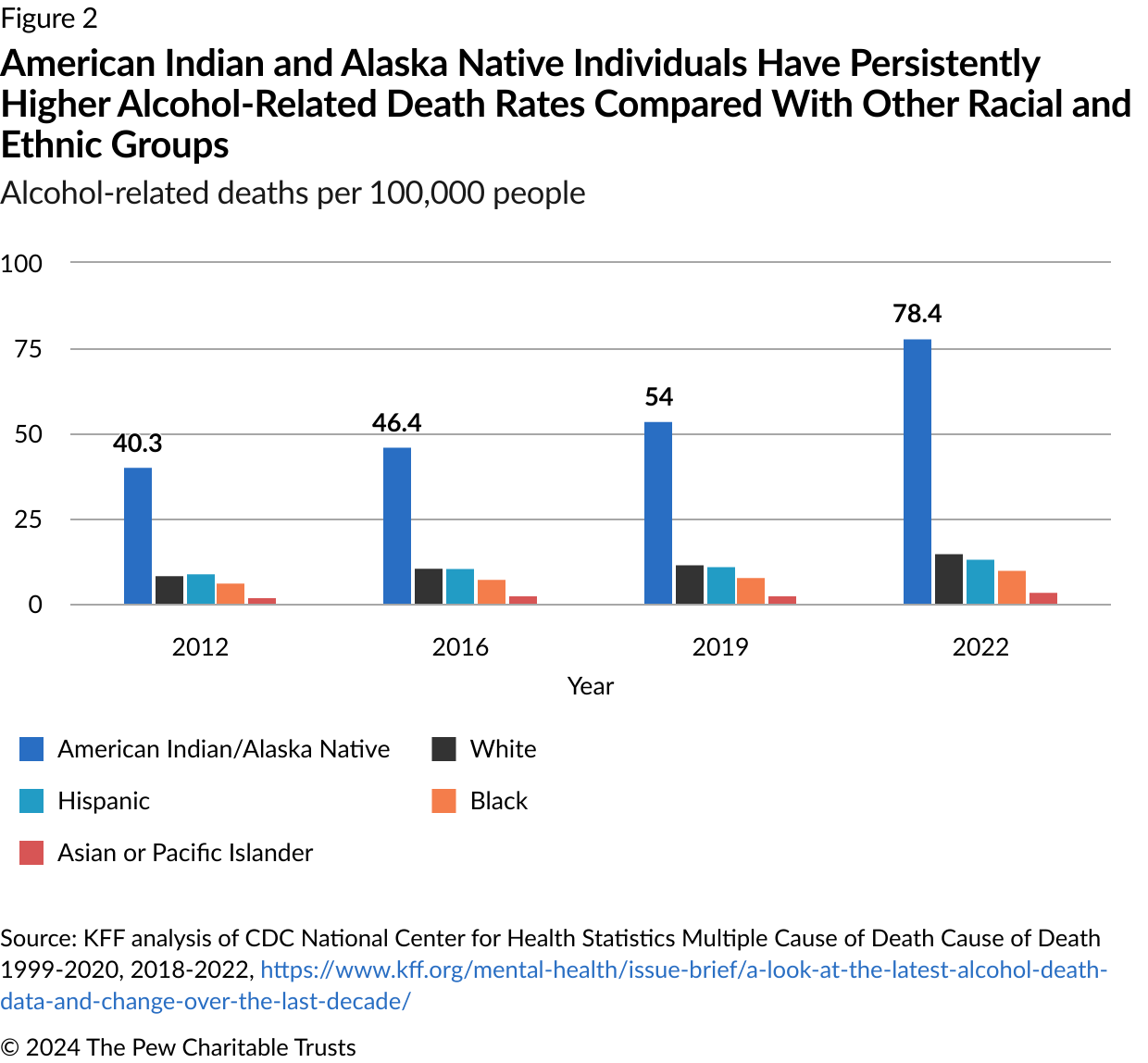
American Indian and Alaska Native communities
Despite seeking treatment at higher rates than other racial/ethnic groups, American Indian and Alaska Native people have the highest rate of alcohol-related deaths.84
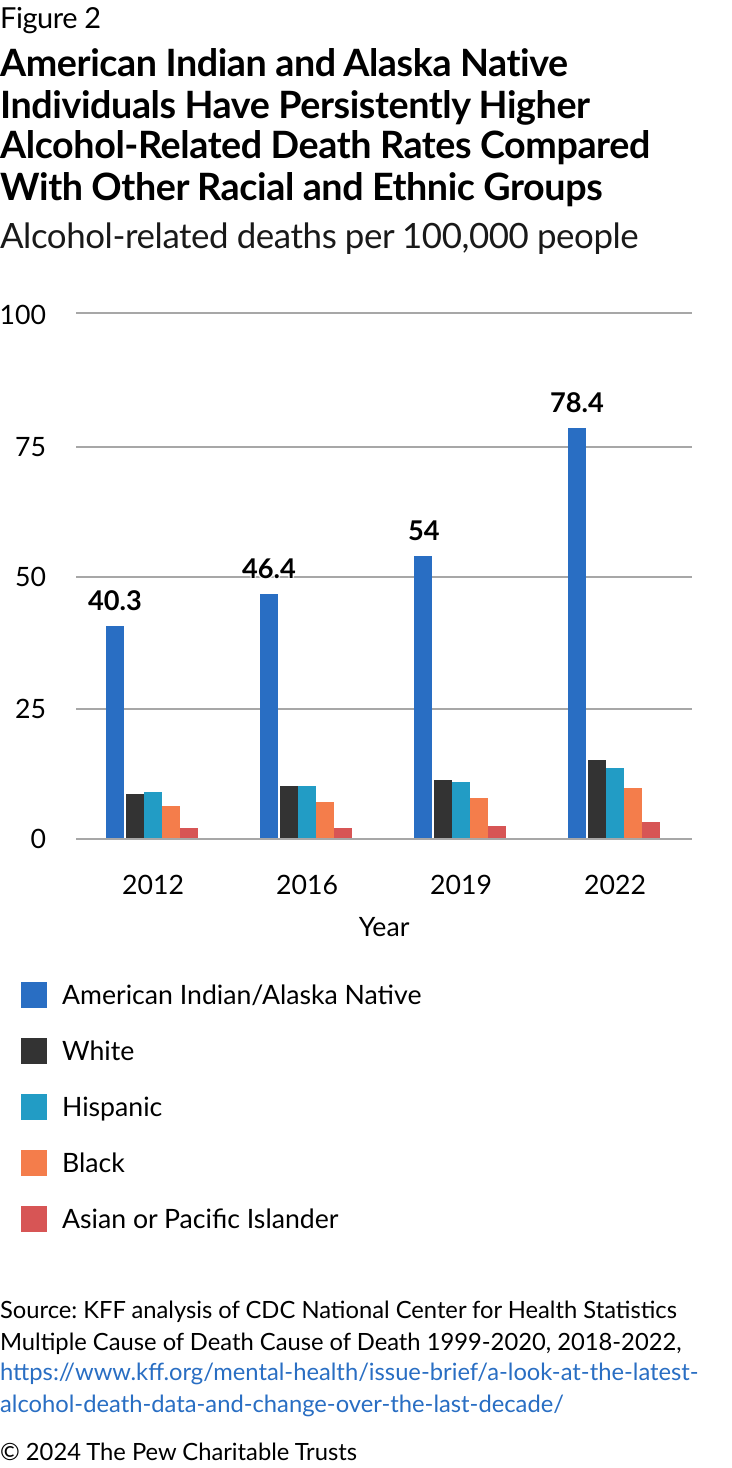
Risk factors that impact these communities and can contribute to these deaths include historical and ongoing trauma from colonization, the challenges of navigating both native and mainstream American cultural contexts, poverty resulting from forced relocation, and higher rates of mental health conditions than in the general population.85 Substances, including alcohol, are sometimes used to cope with these challenges.86
However, American Indian/Alaska Native communities also have rich protective factors such as their cultures, languages, traditions, and connections to elders, which can help reduce negative outcomes associated with alcohol use, especially when treatment services incorporate and build on these strengths.87
For example, interviews with American Indian/Alaska Native patients with AUD in the Pacific Northwest revealed that many participants preferred Native-led treatment environments that incorporated traditional healing practices and recommended the expansion of such services.88
To improve alcohol-related outcomes for American Indians and Alaska Natives, policymakers and health care providers must develop a greater understanding of the barriers and strengths of these diverse communities and support the development of culturally and linguistically appropriate services. The federal Department of Health and Human Services Office of Minority Health defines such an approach as “services that are respectful of and responsive to the health beliefs, practices, and needs of diverse patients.”89
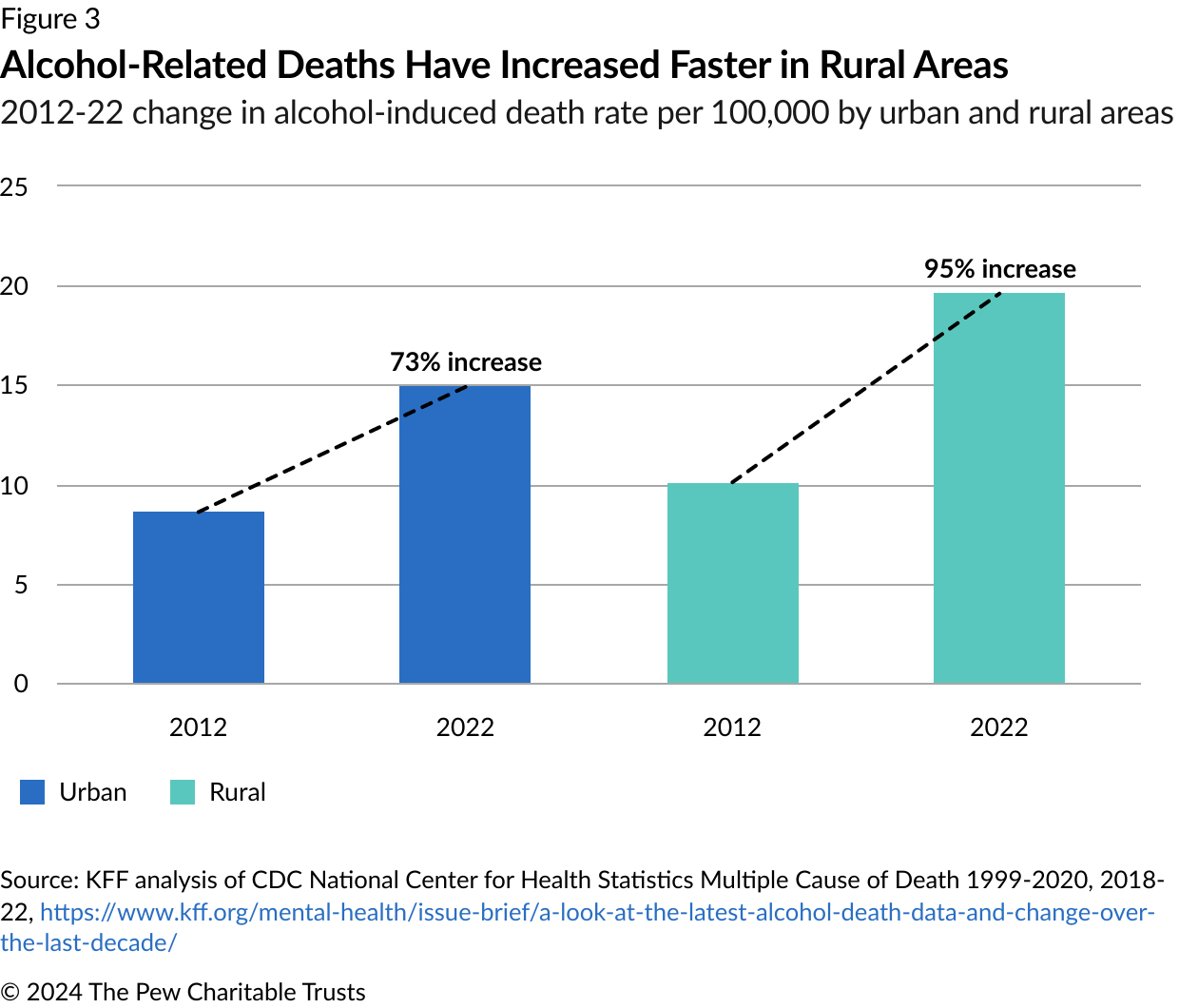
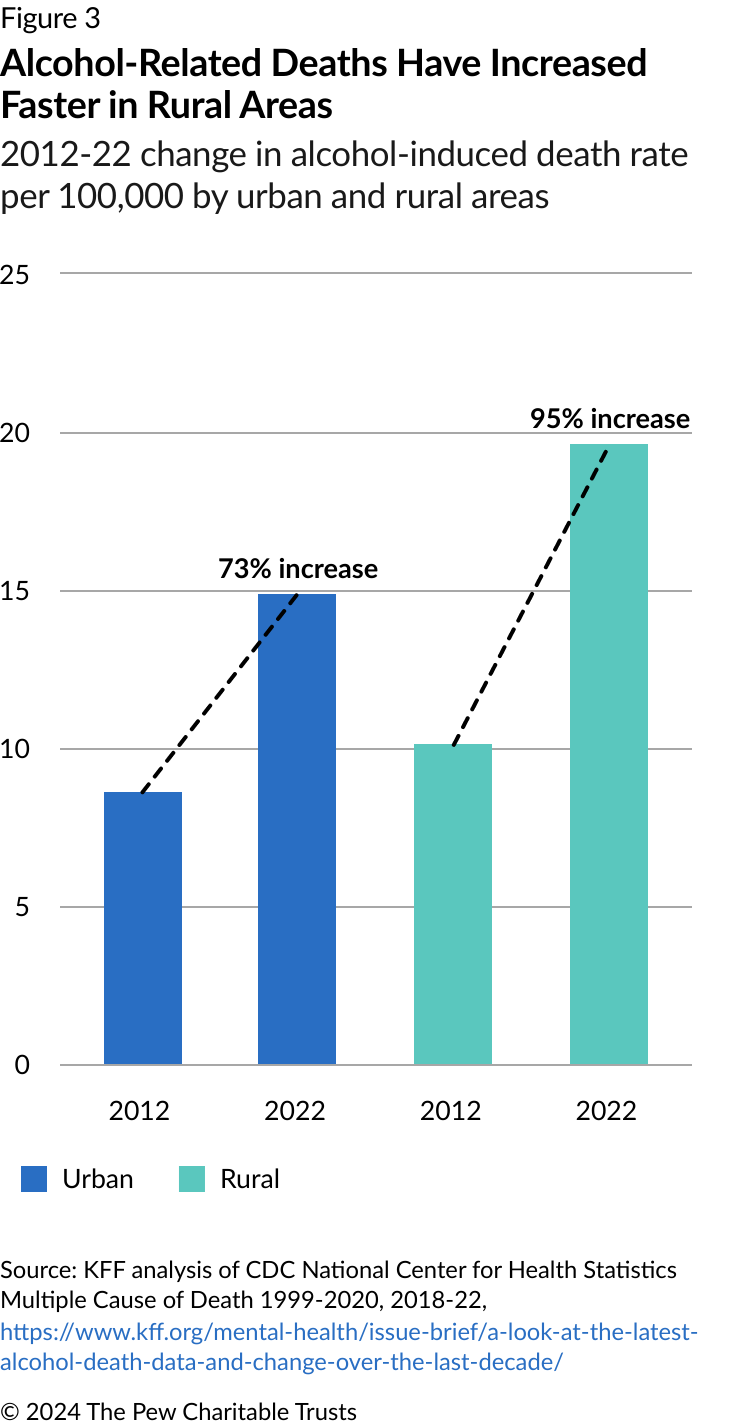
People living in rural areas
Rural communities are another group disproportionately affected by AUD. People living in rural areas have higher alcohol-related mortality rates than urban residents but are often less likely to receive care.90 They face treatment challenges including limited options for care; concerns about privacy while navigating treatment in small, close knit communities; and transportation barriers.91
Telemedicine can help mitigate these barriers to care.92 Cognitive behavioral therapy and medications for AUD can be delivered effectively in virtual settings.93 People with AUD can also benefit from virtual mutual-help meetings, though some find greater value in face-to-face gatherings.94
Despite the value of virtual care delivery, people living in rural areas also often have limited access to broadband internet, which can make these interventions challenging to use.95 Because of this, better access to in-person care is also needed.
Next steps
To improve screening and treatment for patients with AUD, policymakers, payers, and providers should consider strategies to:
- Conduct universal screenings for unhealthy alcohol use and appropriately follow up when those screenings indicate a problem. Less than 20% of people with AUD proactively seek care, so health care providers shouldn’t wait for patients to ask them for help.96
- Connect people with continued care after withdrawal management so that they can begin their recovery. People leaving withdrawal management settings should have a treatment plan that meets their needs—whether that’s behavioral treatment, recovery supports, medication, or a combination of these approaches.
- Further the use of medications for AUD. With just 2% of people with AUD receiving medication, significant opportunities exist to increase utilization and improve outcomes.97
- Address disparities through culturally competent treatment and increased access in rural areas. The populations most impacted by AUD should have access to care that meets their needs and preferences.
AUD is a common and treatable health condition that often goes unrecognized or unaddressed. Policymakers can improve the health of their communities by supporting providers in increasing the use of evidence-based treatment approaches.98
If you are concerned about your alcohol consumption, you can use the Check Your Drinking tool created by the Centers for Disease Control and Prevention to assess your drinking levels and make a plan to reduce your use.
Endnotes
- “Alcohol Use and Your Health,” Centers for Disease Control and Prevention, May 15, 2024, https://www.cdc.gov/alcohol/about-alcohol-use/index.html. National Institute on Alcohol Abuse and Alcoholism, “Alcohol-Related Deaths, Which Increased During the First Year of the COVID-19 Pandemic, Continued to Rise in 2021,” news release, April 12, 2023, https://www.niaaa.nih.gov/news-events/researchupdate/alcohol-related-deaths-which-increased-during-first-year-covid-19-pandemic-continued-rise-2021. Merianne Rose Spencer, Arialdi M. Miniño, and Margaret Warner, “Drug Overdose Deaths in the United States, 2001–2021,” Centers for Disease Control and Prevention, National Center for Health Statistics, 2022, https://www.cdc.gov/nchs/products/databriefs/db457.htm.
- “2022 National Survey on Drug Use and Health: Detailed Tables,” Substance Abuse and Mental Health Services Administration, https://www.samhsa.gov/data/report/2022-nsduh-detailed-tables.
- “Alcohol Use and Your Health,” Centers for Disease Control and Prevention.
- “Risky Alcohol Use: An Epidemic Inside the COVID-19 Pandemic,” National Institutes of Health, July 28, 2023, https://covid19.nih.gov/news-and-stories/risky-drinking-alcohol-use-epidemic-inside-covid-19-pandemic. Aaron M. White et al., “Alcohol-Related Deaths During the COVID-19 Pandemic,” Journal of the American Medical Association 327, no. 17 (2022): 1704-06, https://doi.org/10.1001/jama.2022.4308. White et al. classified deaths as alcohol-related “if an alcohol-induced cause was listed as the underlying cause and/or as a multiple cause of death.” Deaths were categorized according to ICD-10 codes, which include those related to “alcohol overdose,” “mental and behavioral disorders due to use of alcohol, harmful use,” “alcohol-associated liver diseases,” and “other alcohol-induced causes.”
- Substance Abuse and Mental Health Services Administration, “Key Substance Use and Mental Health Indicators in the United States: Results From the 2022 National Survey on Drug Use and Health,” 2023, https://www.samhsa.gov/data/sites/default/files/reports/rpt42731/2022-nsduh-nnr.pdf
- “Alcohol’s Effects on Health: Understanding Alcohol Use Disorder,” National Institute on Alcohol Abuse and Alcoholism, September 2024, https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-use-disorders. “Alcohol Use Disorder,” National Library of Medicine and MedlinePlus, Jan. 1, 2018, https://ghr.nlm.nih.gov/condition/alcohol-use-disorder#genes.
- Brittany Chatterton et al., “Alcohol Screening During U.S. Primary Care Visits, 2014-2016,” Journal of General Internal Medicine 37 (2022): 3848-52, https://doi.org/10.1007/s11606-021-07369-1. Leela Chockalingam, Ellen L. Burnham, and Sarah E. Jolley, “Medication Prescribing for Alcohol Use Disorders During Alcohol-Related Encounters in a Colorado Regional Healthcare System,” Alcohol, Clinical and Experimental Research 46, no. 6 (2022): 1094-102, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9246874/. Samantha J. Harris, Amanda J. Abraham, and Courtney R. Yarbrough, “Availability of Medications for Alcohol Use Disorder Treatment in Medicare Part D, 2014-2018,” Journal of Studies on Alcohol and Drugs 83, no. 5 (2022): 653-61, https://www.jsad.com/doi/abs/10.15288/jsad.21-00411. Paul J. Joudrey et al., “Inpatient Adoption of Medications for Alcohol Use Disorder: A Mixed-Methods Formative Evaluation Involving Key Stakeholders,” Drug and Alcohol Dependence 213 (2020): 108090, https://www.sciencedirect.com/science/article/pii/S0376871620302556. Carrie M. Mintz et al., “A Cascade of Care for Alcohol Use Disorder: Using 2015-2019 National Survey on Drug Use and Health Data to Identify Gaps in Past 12-Month Care,” Alcohol, Clinical and Experimental Research 45, no. 6 (2021): 1276-86, https://doi.org/10.1111/acer.14609.
- Colby J. Hyland et al., “Integration of Pharmacotherapy for Alcohol Use Disorder Treatment in Primary Care Settings: A Scoping Review,” Journal of Substance Abuse Treatment 144 (2023): 108919, https://www.sciencedirect.com/science/article/pii/S074054722200201X. Susan A. Rombouts et al., “Evidence Based Models of Care for the Treatment of Alcohol Use Disorder in Primary Health Care Settings: A Systematic Review,” BMC Family Practice 21, no. 1 (2020): 260, https://doi.org/10.1186/s12875-020-01288-6.
- “About Moderate Alcohol Use,” Centers for Disease Control and Prevention, May 15, 2024, https://www.cdc.gov/alcohol/about-alcohol-use/moderate-alcohol-use.html.
- “About Standard Drink Sizes,” Centers for Disease Control and Prevention, May 15, 2024, https://www.cdc.gov/alcohol/standard-drink-sizes/index.html.
- “Alcohol Use and Your Health,” Centers for Disease Control and Prevention.
- “Alcohol Use and Your Health,” Centers for Disease Control and Prevention.
- Sara A. Nehring, Richard J. Chen, and Andrew M. Freeman, “Alcohol Use Disorder,” StatPearls [Internet], https://www.ncbi.nlm.nih.gov/books/NBK436003/.
- “Alcohol Use Disorder: A Comparison Between DSM-IV and DSM-5,” National Institute on Alcohol Abuse and Alcoholism, April 2021, https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-use-disorder-comparison-between-dsm.
- Sara A. Nehring, Richard J. Chen, and Andrew M. Freeman, “Alcohol Use Disorder.”
- Virginia A. Moyer, “Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse: U.S. Preventive Services Task Force Recommendation Statement,” Annals of Internal Medicine 159, no. 3 (2013): 210-18, https://www.acpjournals.org/doi/full/10.7326/0003-4819-159-3-201308060-00652. Carrie M. Mintz et al., “A Cascade of Care for Alcohol Use Disorder: Using 2015-2019 National Survey.”
- “Screening, Brief Intervention, and Referral to Treatment (SBIRT),” Substance Abuse and Mental Health Services Administration, Aug. 12, 2022, https://www.samhsa.gov/sbirt
- American Public Health Association and Education Development Center Inc., “Alcohol Screening and Brief Intervention: A Guide for Public Health Practitioners,” 2008, https://www.lifespan.org/sites/default/files/lifespan-files/documents/centers/injury-prevention-center/alcohol-screeening-and-brief-intervention-web.pdf. Elizabeth A. O’Connor et al., “Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: Updated Evidence Report and Systematic Review for the U.S. Preventive Services Task Force,” JAMA 320, no. 18 (2018): 1910-28, https://jamanetwork.com/journals/jama/fullarticle/2714536
- “Core Resource on Alcohol: About the Core Resource on Alcohol,” National Institute on Alcohol Abuse and Alcoholism, https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/about-core-resource-alcohol.
- Felicia W. Chi et al., “Alcohol Brief Intervention, Specialty Treatment and Drinking Outcomes at 12 Months: Results From a Systematic Alcohol Screening and Brief Intervention Initiative in Adult Primary Care,” Drug and Alcohol Dependence 235 (2022): 109458, https://www.sciencedirect.com/science/article/pii/S0376871622001958. Ethan Sahker et al., “Screening, Brief Intervention, and Referral to Treatment Demonstrates Effectiveness in Reducing Drinking in a Midwest American Service Sample,” International Journal of Mental Health and Addiction 18 (2020): 138-48, https://link.springer.com/article/10.1007/s11469-018-9953-1.
- Carrie M. Mintz et al., “A Cascade of Care for Alcohol Use Disorder: Using 2015-2019 National Survey.”
- Carrie M. Mintz et al., “A Cascade of Care for Alcohol Use Disorder: Using 2015-2019 National Survey.""
- John G. Roubil et al., “Assessing Screening, Brief Intervention, and Referral to Treatment (SBIRT) Compliance and Disparities for Pediatric Inpatients at a Tertiary Care Facility,” Journal of Pediatric Surgery 57, no. 1 (2022): 111-6, https://www.sciencedirect.com/science/article/pii/S0022346821006667.
- Marissa B. Esser et al., “Trends in Emergency Department Visits Related to Acute Alcohol Consumption Before and During the COVID-19 Pandemic in the United States, 2018-2020,” Drug and Alcohol Dependence Reports 3 (2022): 100049, https://www.sciencedirect.com/science/article/pii/S2772724622000270?via%3Dihub. Substance Abuse and Mental Health Services Administration, “Short Report: Alcohol-Related ED Visits,” 2024, https://www.samhsa.gov/data/sites/default/files/reports/rpt44498/DAWN-TargetReportAlcohol-508.pdf
- Isabel A. Barata et al., “Effectiveness of SBIRT for Alcohol Use Disorders in the Emergency Department: A Systematic Review,” Western Journal of Emergency Medicine 18, no. 6 (2017): 1143-52, https://escholarship.org/uc/item/60s175hz.
- Isabel A. Barata et al., “Effectiveness of SBIRT for Alcohol Use Disorders.”
- Janice Vendetti et al., “Screening, Brief Intervention, and Referral to Treatment (SBIRT): Implementation Barriers, Facilitators, and Model Migration,” Addiction 112, no. S2 (2017): 23-33, https://onlinelibrary.wiley.com/doi/abs/10.1111/add.13652.
- Amanda M. Bunting et al., “Characteristics of Substance Use Screening at Intake in a Sample of U.S. Jails,” Journal of Health Care for the Poor and Underserved 34, no. 1 (2023): 180-91, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10938471/.
- “Alcohol Use Disorder: From Risk to Diagnosis to Recovery,” National Institute on Alcohol Abuse and Alcoholism, Feb. 27, 2024, https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/alcohol-use-disorder-risk-diagnosis-recovery
- “Alcohol Use Disorder: From Risk to Diagnosis to Recovery,” National Institute on Alcohol Abuse and Alcoholism.
- “Alcohol Use Disorder: From Risk to Diagnosis to Recovery,” National Institute on Alcohol Abuse and Alcoholism.
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline on Alcohol Withdrawal Management,” 2020, https://downloads.asam.org/sitefinity-production-blobs/docs/default-source/quality-science/the_asam_clinical_practice_guideline_on_alcohol-1.pdf?sfvrsn=ba255c2_0. Ed Day and Chris Daly, “Clinical Management of the Alcohol Withdrawal Syndrome,” Addiction 117, no. 3 (2021): 804-14, https://onlinelibrary.wiley.com/doi/abs/10.1111/add.15647.
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline.”
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline.”
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline.”
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline.”
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline.”
- American Society of Addiction Medicine, “The ASAM Clinical Practice Guideline.”
- Bureau of Justice Assistance and National Institute of Corrections, “Guidelines for Managing Substance Withdrawal in Jails,” 2023, https://www.cossup.org/Content/Documents/JailResources/Guidelines_for_Managing_Substance_Withdrawal_in_Jails_6-6-23_508.pdf.
- Margaret T. Lee et al., “A Performance Measure for Continuity of Care After Detoxification: Relationship With Outcomes,” Journal of Substance Abuse Treatment 47, no. 2 (2014): 130-39, https://doi.org/10.1016/j.jsat.2014.04.002.
- Todd Molfenter, Jee-Seon Kim, and Mark Zehner, “Increasing Engagement in Post-Withdrawal Management Services Through a Practice Bundle and Checklist,” The Journal of Behavioral Health Services & Research 48, no. 3 (2021): 400-09, https://doi.org/10.1007/s11414-020-09700-w.
- Christine Timko et al., “Transitioning From Detoxification to Substance Use Disorder Treatment: Facilitators and Barriers,” Journal of Substance Abuse Treatment 70 (2016): 64-72, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6448765/.
- Allison R. David et al., “Barriers to Accessing Treatment for Substance Use After Inpatient Managed Withdrawal (Detox): A Qualitative Study,” Journal of Substance Abuse Treatment 142 (2022): 108870, https://doi.org/10.1016/j.jsat.2022.108870.
- Margaret T. Lee et al., “Impact of Recovery Support Navigators on Continuity of Care After Detoxification,” Journal of Substance Abuse Treatment 112 (2020): 10-16, https://doi.org/10.1016/j.jsat.2020.01.019. Nicholas Livingston et al., “Interventions to Improve Post Detoxification Treatment Engagement and Alcohol Recovery: Systematic Review of Intervention Types and Effectiveness,” Alcohol and Alcoholism 57, no. 1 (2021): 136-50, https://doi.org/10.1093/alcalc/agab021. Todd Molfenter, Jee-Seon Kim, and Mark Zehner, “Increasing Engagement in Post-Withdrawal Management Services.”
- “Alcohol Use Disorder (AUD) in the United States: Age Groups and Demographic Characteristics,” National Institute on Alcohol Abuse and Alcoholism, 2024, https://www.niaaa.nih.gov/alcohols-effects-health/alcohol-topics/alcohol-facts-and-statistics/alcohol-usedisorder-aud-united-states-age-groups-and-demographic-characteristics.
- Lara A. Ray et al., “State-of-the-Art Behavioral and Pharmacological Treatments for Alcohol Use Disorder,” The American Journal of Drug and Alcohol Abuse 45, no. 2 (2019): 124-40, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6430676/.
- 47 Dianna M. Wolfe et al., “Service-Level Barriers to and Facilitators of Accessibility to Treatment for Problematic Alcohol Use: A Scoping Review,” Frontiers in Public Health 11 (2023): 1296239, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10722420/. Alexandra Venegas et al., “Understanding Low Treatment Seeking Rates for Alcohol Use Disorder: A Narrative Review of the Literature and Opportunities for Improvement,” The American Journal of Drug and Alcohol Abuse 47, no. 6 (2021): 664-79, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9059657/.
- Susan A. Rombouts et al., “Evidence Based Models of Care for the Treatment of Alcohol Use Disorder.”
- Katrin Charlet and Andreas Heinz, “Harm Reduction—a Systematic Review on Effects of Alcohol Reduction on Physical and Mental Symptoms,” Addiction Biology 22, no. 5 (2017): 1119-59, https://onlinelibrary.wiley.com/doi/abs/10.1111/adb.12414.
- Susan A. Rombouts et al., “Evidence Based Models of Care for the Treatment of Alcohol Use Disorder.”
- Agency for Healthcare Research and Quality, “Pharmacotherapy for Adults With Alcohol Use Disorder in Outpatient Settings: Systematic Review,” 2023, https://effectivehealthcare.ahrq.gov/products/alcohol-use-disorders/research#field_report_title_3. Eden Y. Bernstein et al., “Outcomes After Initiation of Medications for Alcohol Use Disorder at Hospital Discharge,” JAMA Network Open 7, no. 3 (2024):e243387, https://doi.org/10.1001/jamanetworkopen.2024.3387
- Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism, “Medication for the Treatment of Alcohol Use Disorder: A Brief Guide,” 2015, https://store.samhsa.gov/sites/default/files/sma15-4907.pdf.
- Substance Abuse and Mental Health Services Administration, “Results From the 2022 National Survey on Drug Use and Health.”
- Matheus Cheibub David Marin et al., “Pharmacological Treatment of Alcohol Cravings,” Brain Sciences 13, no. 8 (2023): 1206, https://www.mdpi.com/2076-3425/13/8/1206.
- The American Psychiatric Association, Practice Guideline for the Pharmacological Treatment of Patients With Alcohol Use Disorder (American Psychiatric Association Publishing, 2018), https://psychiatryonline.org/doi/book/10.1176/appi.books.9781615371969.
- Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism, “Medication for the Treatment of Alcohol Use Disorder.” Glenn-Milo Santos et al., “Targeted Oral Naltrexone for Mild to Moderate Alcohol Use Disorder Among Sexual and Gender Minority Men: A Randomized Trial,” The American Journal of Psychiatry 179, no. 12 (2022): 915-26, https://ajp.psychiatryonline.org/doi/abs/10.1176/appi.ajp.20220335.
- Agency for Healthcare Research and Quality, “Pharmacotherapy for Adults With Alcohol Use Disorder in Outpatient Settings.”
- Agency for Healthcare Research and Quality, “Pharmacotherapy for Adults With Alcohol Use Disorder in Outpatient Settings.”
- Augustin G. L. Vannier et al., “Incidence and Progression of Alcohol-Associated Liver Disease After Medical Therapy for Alcohol Use Disorder,” JAMA Network Open 5, no. 5 (2022): e2213014, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2792500
- Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism, “Medication for the Treatment of Alcohol Use Disorder.”
- Daniel E. Jonas et al., “Pharmacotherapy for Adults With Alcohol Use Disorders in Outpatient Settings: A Systematic Review and Meta Analysis,” JAMA 311, no. 18 (2014): 1889-1900, https://www.ncbi.nlm.nih.gov/pubmed/24825644.
- Agency for Healthcare Research and Quality, “Pharmacotherapy for Adults With Alcohol Use Disorder in Outpatient Settings.”
- The American Psychiatric Association, Practice Guideline for the Pharmacological Treatment
- Substance Abuse and Mental Health Services Administration and National Institute on Alcohol Abuse and Alcoholism, “Medication for the Treatment of Alcohol Use Disorder.”
- Agency for Healthcare Research and Quality, “Pharmacotherapy for Adults With Alcohol Use Disorder in Outpatient Settings.”
- George F. Koob, “Alcohol Use Disorder Treatment: Problems and Solutions,” Annual Review of Pharmacology and Toxicology 64 (2024): 255-75, https://www.annualreviews.org/content/journals/10.1146/annurev-pharmtox-031323-115847
- George F. Koob, “Alcohol Use Disorder Treatment: Problems and Solutions.”
- Agency for Healthcare Research and Quality, “Pharmacotherapy for Adults With Alcohol Use Disorder in Outpatient Settings.” Barbara J. Mason and Charles J. Heyser, “Alcohol Use Disorder: The Role of Medication in Recovery,” Alcohol Research: Current Reviews 41, no. 1 (2021): https://arcr.niaaa.nih.gov/volume/41/1/alcohol-use-disorder-role-medication-recovery
- Augustin G. L. Vannier et al., “Incidence and Progression of Alcohol-Associated Liver Disease.”
- Caroline Gregory et al., “First-Line Medications for the Outpatient Treatment of Alcohol Use Disorder: A Systematic Review of Perceived Barriers,” Journal of Addiction Medicine 16, no. 4 (2022): e210-e218, https://pubmed.ncbi.nlm.nih.gov/34561352/.
- The Stages of Change Model posits that individuals move through five stages of change: precontemplation, contemplation, preparation, action, and maintenance
- Mary E. McCaul and Nancy M. Petry, “The Role of Psychosocial Treatments in Pharmacotherapy for Alcoholism,” The American Journal on Addictions 12, no. s1 (2003): s41-s52, https://www.ncbi.nlm.nih.gov/pubmed/14972779. James O. Prochaska, Carlo C. DiClemente, and John C. Norcross, “In Search of How People Change: Applications to Addictive Behaviors,” American Psychologist 47, no. 9 (1992): 1102-14, https://www.avannistelrooij.nl/wp-content/uploads/2024/05/Prochaska-ea-1992-how-people-change-AP-1.pdf. J.D. Sellman et al., “A Randomized Controlled Trial of Motivational Enhancement Therapy (MET) for Mild to Moderate Alcohol Dependence,” Journal of Studies on Alcohol and Drugs 62, no. 3 (2001): 389-96, https://www.ncbi.nlm.nih.gov/pubmed/11414349. Eirini I. Vasilaki, Steven G. Hosier, and W. Miles Cox, “The Efficacy of Motivational Interviewing as a Brief Intervention for Excessive Drinking: A Meta-Analytic Review,” Alcohol and Alcoholism 41, no. 3 (2006): 328-35, https://www.ncbi.nlm.nih.gov/pubmed/16547122.
- Molly Magill and Lara A. Ray, “Cognitive-Behavioral Treatment With Adult Alcohol and Illicit Drug Users: A Meta-Analysis of Randomized Controlled Trial,” Journal of Studies on Alcohol and Drugs 70, no. 4 (2009): 516-27, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696292/. Mary E. McCaul and Nancy M. Petry, “The Role of Psychosocial Treatments in Pharmacotherapy.”
- Julianne C. Flanagan et al., “Behavioral Treatments for Alcohol Use Disorder and Post-Traumatic Stress Disorder,” Alcohol Research Current Reviews 39, no. 2 (2018): 181-92, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6561400/.
- Lara A. Ray et al., “State-of-the-Art Behavioral and Pharmacological Treatments.”
- Lara A. Ray et al., “State-of-the-Art Behavioral and Pharmacological Treatments.”
- Lara A. Ray et al., “State-of-the-Art Behavioral and Pharmacological Treatments.”
- Substance Abuse and Mental Health Services Administration, “Value of Peers, 2017,” 2017, https://www.samhsa.gov/sites/default/files/programs_campaigns/brss_tacs/value-of-peers-2017.pdf
- Maria J. O’Connell et al., “Enhancing Outcomes for Persons With Co-Occurring Disorders Through Skills Training and Peer Recovery Support,” Journal of Mental Health 29, no. 1 (2017): 6-11, https://doi.org/10.1080/09638237.2017.1294733. Michael Rowe et al., “A PeerSupport, Group Intervention to Reduce Substance Use and Criminality Among Persons With Severe Mental Illness,” Psychiatric Services 58, no. 7 (2007): 955-61, https://www.ncbi.nlm.nih.gov/pubmed/17602012.
- John F. Kelly and Julie D. Yeterian, “The Role of Mutual-Help Groups in Extending the Framework of Treatment,” Alcohol Research and Health 33, no. 4 (2011): 350-55, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860535/.
- John F. Kelly and Julie D. Yeterian, “The Role of Mutual-Help Groups.”
- Alyssa T. Brooks et al., “A Qualitative Exploration of Social Support During Treatment for Severe Alcohol Use Disorder and Recovery,” Addictive Behaviors Reports 6 (2017): 76-82, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5800591/. K. Witkiewitz, R.Z. Litten, and L. Leggio, “Advances in the Science and Treatment of Alcohol Use Disorder,” Science Advances 5, no. 9 (2019): eaax4043, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6760932/.
- Marissa B. Esser et al., “Deaths From Excessive Alcohol Use—United States, 2016-2021,” Morbidity and Mortality Weekly Report 73, no. 8 (2024): 154-61, https://www.cdc.gov/mmwr/volumes/73/wr/mm7308a1.htm.
- Marc A. Emerson, Roland S. Moore, and Raul Caetano, “Correlates of Alcohol-Related Treatment Among American Indians and Alaska Natives With Lifetime Alcohol Use Disorder,” Alcohol, Clinical and Experimental Research 43, no. 1 (2019): 115-22, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6318056. Ibraheem M. Karaye, Nasim Maleki, and Ismaeel Yunusa, “Racial and Ethnic Disparities in AlcoholAttributed Deaths in the United States, 1999-2020,” International Journal of Environmental Research and Public Health 20, no. 8 (2023): 5587, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10138663/.
- Claradina Soto et al., “Substance and Behavioral Addictions Among American Indian and Alaska Native Populations,” International Journal of Environmental Research and Public Health 19, no. 5 (2022): 2974, https://www.mdpi.com/1660-4601/19/5/2974.
- Claradina Soto et al., “Substance and Behavioral Addictions Among American Indian and Alaska Native Populations.”
- Claradina Soto et al., “Substance and Behavioral Addictions Among American Indian and Alaska Native Populations.”
- Lonnie A. Nelson et al., “Content Analysis of Preferred Recovery Pathways Among Urban American Indians and Alaska Natives Experiencing Alcohol Use Disorders,” Journal of Cross-Cultural Psychology 54, no. 1 (2022): 142-60, https://journals.sagepub.com/doi/abs/10.1177/00220221221132778.
- “Cultural and Linguistic Competency,” U.S. Department of Health and Human Services Office of Minority Health, Aug. 8, 2024, https://minorityhealth.hhs.gov/cultural-and-linguistic-competency
- Christal N. Davis and Susan E. O’Neill, “Treatment of Alcohol Use Problems Among Rural Populations: A Review of Barriers and Considerations for Increasing Access to Quality Care,” Current Addiction Reports 9 (2022): 432-44, https://link.springer.com/article/10.1007/s40429-022-00454-3.
- Christal N. Davis and Susan E. O’Neill, “Treatment of Alcohol Use Problems Among Rural Populations: A Review.”
- Christal N. Davis and Susan E. O’Neill, “Treatment of Alcohol Use Problems Among Rural Populations: A Review.” Arpad Kelemen et al., “Telehealth Interventions for Alcohol Use Disorder: A Systematic Review,” Liver Research 6, no. 3 (2022): 146-54, https://www.sciencedirect.com/science/article/pii/S254256842200040X. Ponni V. Perumalswami et al., “Telehealth and Delivery of Alcohol Use Disorder Treatment in the Veterans Health Administration,” Alcohol, Clinical and Experimental Research 48, no. 5 (2024): 944-54, https://onlinelibrary.wiley.com/doi/abs/10.1111/acer.15305.
- Kevin A. Hallgren et al., “Treatment Retention and Reductions in Blood Alcohol Concentration (BAC) During the First 90 Days of a Telehealth Program for Alcohol Use Disorder,” The American Journal of Drug and Alcohol Abuse 49, no. 2 (2023): 249-59, https://doi.org/10.1080/00952990.2023.2175322. Arpad Kelemen et al., “Telehealth Interventions for Alcohol Use Disorder.” Ponni V. Perumalswami et al., “Telehealth and Delivery of Alcohol Use Disorder Treatment in the Veterans Health Administration.”
- 4 Evan Senreich et al., “The Experiences of 12-Step Program Attendees Transitioning to Online Meetings During the COVID-19 Pandemic,” Alcoholism Treatment Quarterly 40, no. 4 (2022): 500-17, https://doi.org/10.1080/07347324.2022.2102456. Christine Timko et al., “Mode of Mutual-Help Group Attendance: Predictors and Outcomes in a U.S. National Longitudinal Survey of Adults With Lifetime Alcohol Use Disorder,” Journal of Substance Use and Addiction Treatment 164 (2024): 209395, https://www.sciencedirect.com/science/article/pii/S2949875924001073.
- Kelly A. Hirko et al., “Telehealth in Response to the COVID-19 Pandemic: Implications for Rural Health Disparities,” Journal of the American Medical Informatics Association 27, no. 11 (2020): 1816-18, https://doi.org/10.1093/jamia/ocaa156. “Broadband Access Still a Challenge in Rural Affordable Housing,” Anna Read and Kelly Wert, The Pew Charitable Trusts, Dec. 8, 2022, https://www.pewtrusts.org/en/research-and-analysis/articles/2022/12/08/broadband-access-still-a-challenge-in-rural-affordable-housing.
- Lara A. Ray et al., “State-of-the-Art Behavioral and Pharmacological Treatments.”
- Substance Abuse and Mental Health Services Administration, “Results From the 2022 National Survey on Drug Use and Health.”
- “Alcohol Use Disorder: A Comparison Between DSM-IV and DSM-5,” National Institute on Alcohol Abuse and Alcoholism