U.S. National Trends and Disparities in Suicidal Ideation, Suicide Attempts, and Health Care Use
Low mental health care uptake among high-risk groups including young adults, Black and multiracial adults
Overview
From 2000 to 2020, the overall rate of suicide increased 30% and climbed to more than 49,000 deaths in 2022—the highest number ever recorded in the United States. Suicidal ideation (a range of contemplations, wishes, and preoccupations with death and suicide) and behaviors (which include suicide plans and attempts) not only can lead to suicide deaths but also are important public health issues themselves. For every death by suicide in 2022, about 32 people attempted suicide and more than 250 people seriously considered it. Aggregate numbers, however, mask distinct differences among demographic subgroups.
To better understand the trends and disparities in suicidal thoughts and behaviors among demographic subgroups, The Pew Charitable Trusts worked with Dr. Hillary Samples to analyze 2015-19 data from the National Survey on Drug Use and Health (NSDUH). This research sought to identify risk factors for suicidal ideation and attempts across a comprehensive set of sociodemographic, behavioral, and clinical characteristics. Researchers also looked at how people who experience suicidal ideation interact with the health care system in order to identify opportunities for suicide risk screening and reach more people who need suicide care.
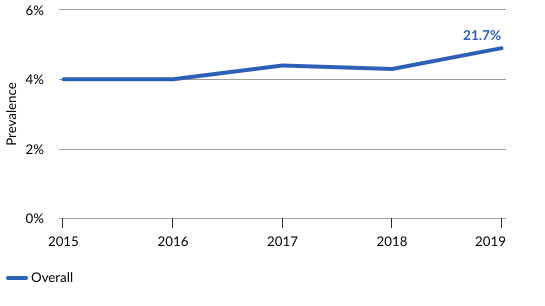
Published in the journal Psychiatric Services, the study produced several key findings. Among adults who reported suicidal ideation, there was a 48% increase in prevalence of suicide attempts among Black adults and an 82% increase among people identifying as more than one race or ethnicity, compared with a nearly 33% decrease in attempts among White adults. Prevalence of suicidal ideation increased by nearly 22% overall, with a pronounced increase of nearly 45% for young adults ages 18-25.
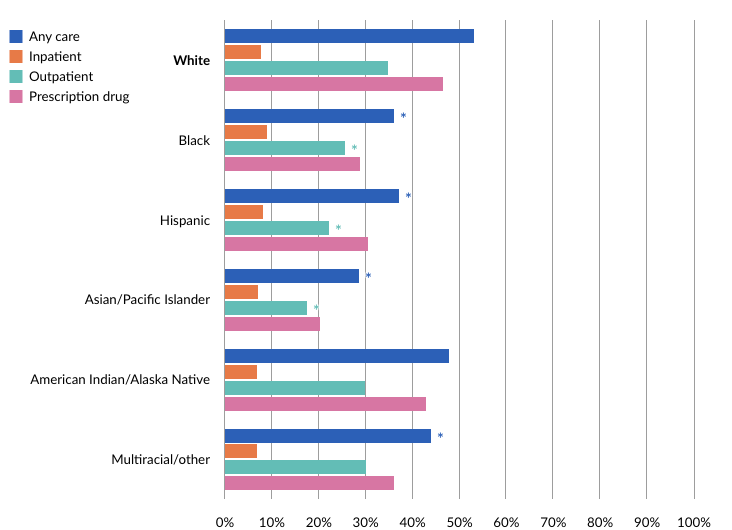
The research also revealed that among people reporting ideation, there was a nearly 87% likelihood that they had received general health care but only a 48% likelihood for mental health care. This discrepancy is significant because accredited mental health care settings are required to screen all patients for suicide risk but accredited general health care settings are not, unless the patient is primarily seeking care for mental health conditions. The findings underscore that general health settings have a prime opportunity to identify more people who are thinking about suicide or planning a suicide attempt and connect them to appropriate care.
Use the interactive tools below to explore the research results further. The data is disaggregated by sex, age, race/ethnicity, education, employment, income, insurance, marital status, sexual orientation, and urbanicity (the degree to which a geographical area is considered urban). Data on health care utilization for people experiencing suicidal ideation is disaggregated by sex, age, and race/ethnicity. Some data adjust, or control, for individual sociodemographic, behavioral (substance use), and clinical (health) characteristics. Details are provided in the notes and the methodology appendix.
Part I: Likelihood of past-year suicidal ideation and suicide attempts over time
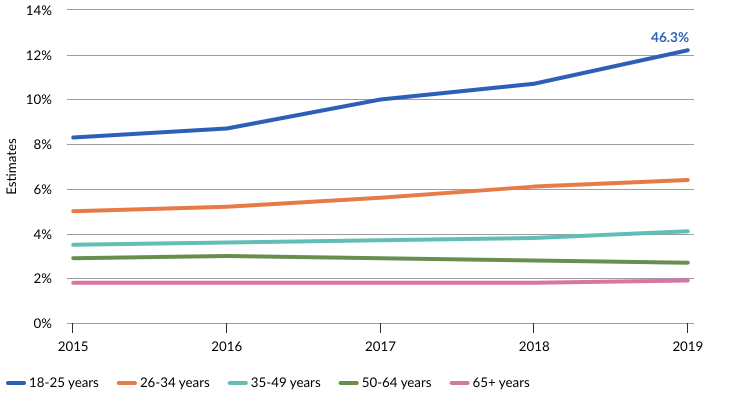
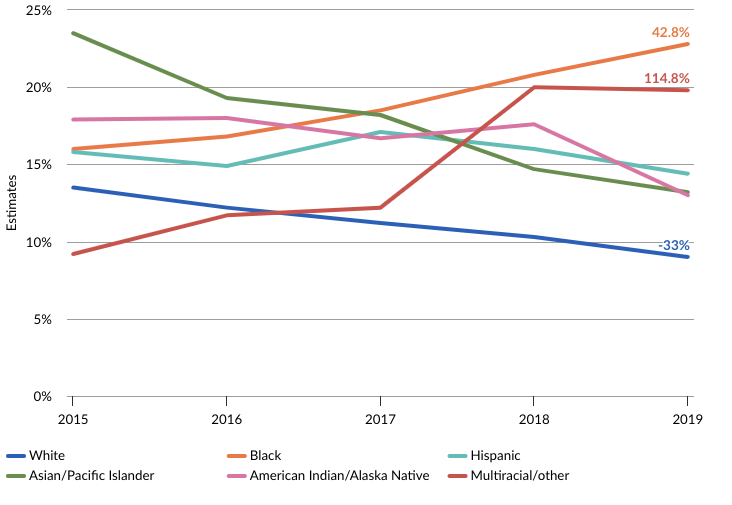
The following interactives show how the likelihood of suicide risk changes over time for age and race/ethnicity groups after adjusting for all other sociodemographic, substance use, and clinical characteristics. These results highlight that there was a significant increase in the likelihood of 18-to-25-year-olds experiencing suicidal ideation, and significant increases in the likelihood of suicide attempts for Black and multiracial/other groups from 2015 to 2019.
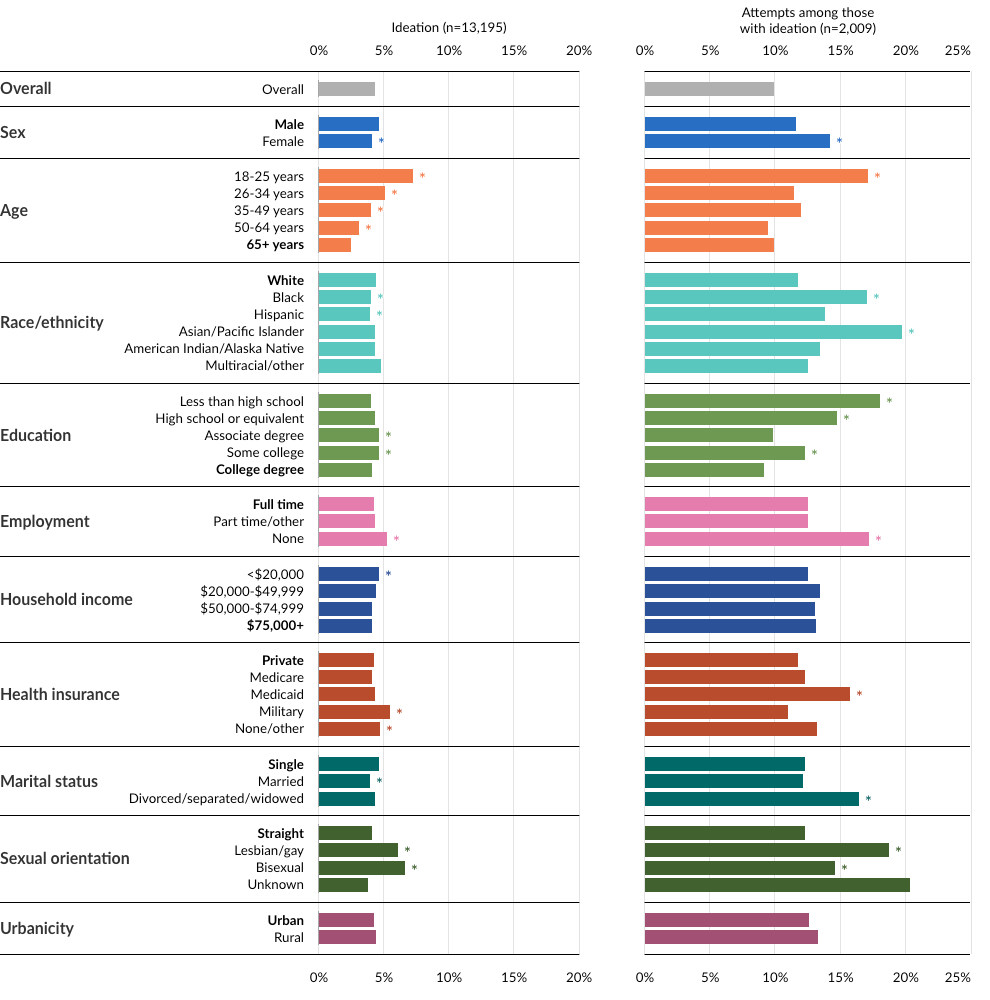
Part II: Likelihood of past-year suicidal ideation and suicide attempts
By utilizing statistical models (see Methodology Appendix), the interactives in this section present suicide risk as the probability, or likelihood, that groups experience past-year ideation and attempts in comparison with a reference group—generally the demographic with the most respondents—for each category (see glossary). Statistical models with categorical variables (e.g., sex, race/ethnicity, age) require one of the categories to be a reference group with which all other groups are compared. These models concurrently controlled or adjusted for the effects of key sociodemographic characteristics, past-year substance use, and health status. The data is helpful to understand differences in suicide risk across subgroups.
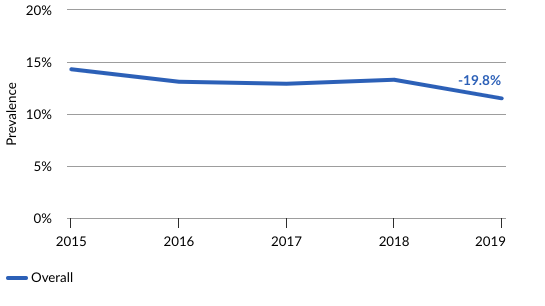
Part III: Prevalence trends in past-year suicidal ideation and attempts
Prevalence trends data shows how the proportion of the population with suicidal ideation and suicide attempts evolves over time. The following interactive illustrates the prevalence of suicidal ideation and attempts from 2015 to 2019 among key sociodemographic subgroups of U.S. adults ages 18 and older, highlighting the increasing risk for certain subgroups. While the graphs examine trends in prevalence for each sociodemographic characteristic separately, they do not directly compare prevalence for different groups nor account for how risk may change when all the sociodemographic characteristics are considered concurrently.
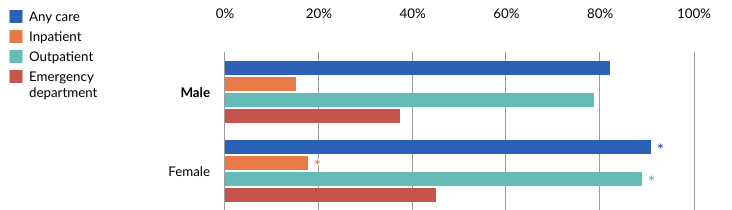
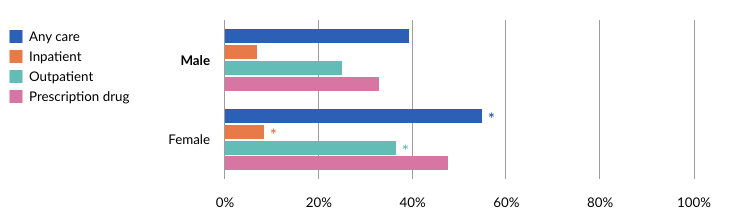
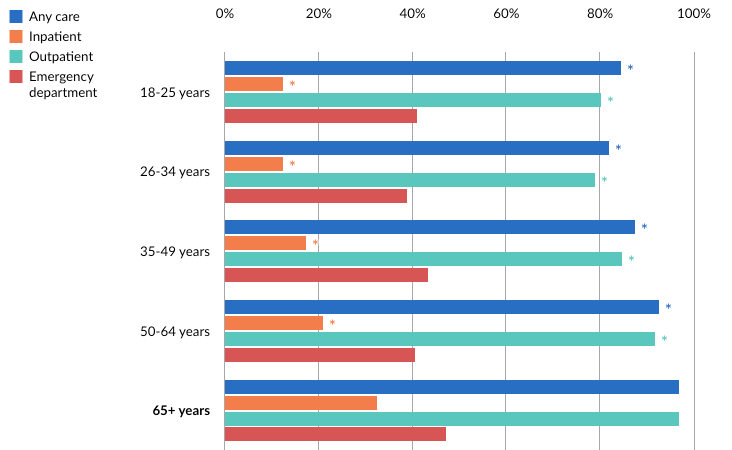
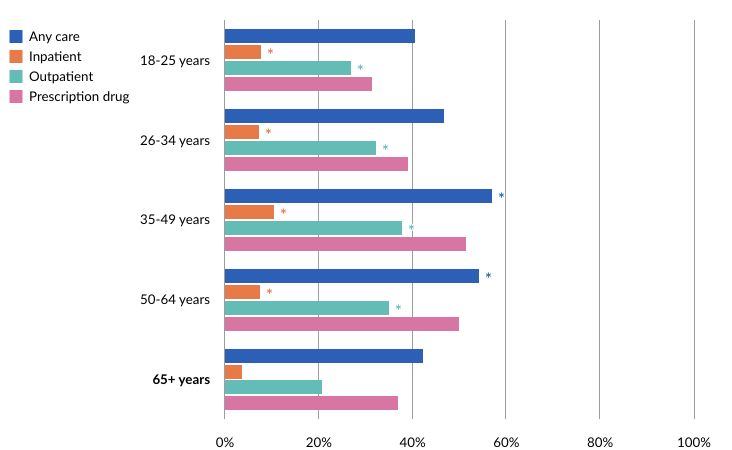
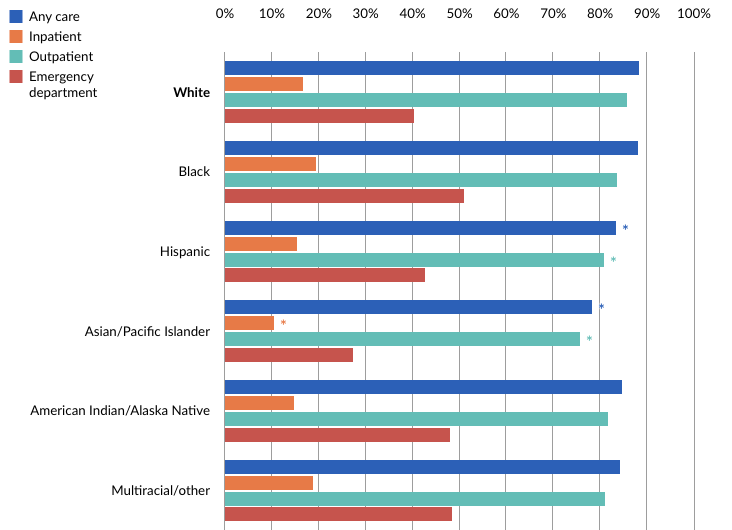
Part IV: Health care utilization among adults with suicidal ideation
The following interactive shows how individuals of different sociodemographic groups experiencing suicidal ideation used either general health care (i.e., inpatient, outpatient, emergency department) or mental health care (i.e., inpatient, outpatient, prescription drug services) in the past year. Understanding how these groups engage with the health care system can help providers better identify opportunities for suicide prevention in clinical settings. This data shows that individuals at risk for suicide are less likely to interact with mental health settings than general health settings, indicating that intervention within general health settings may help patients experiencing suicide risk.
Conclusion
Suicide deaths reached record levels in 2022, indicating the urgent need to better understand and address suicide risk. This study highlighted heightened risk for certain populations, including young people and marginalized racial/ethnic groups. Specifically, findings show overall increases for suicidal ideation with pronounced increasing trends for young adults (ages 18-25). Further, suicide attempts sharply increased among Black and multiracial/other adults compared with a decreasing trend among White adults.
Additional research with larger samples of the marginalized populations is needed to better understand the increasing disparities in risk for these groups, including how risk evolves at the intersection of these identities, such as young Black adults. With more young adults thinking about suicide and widening racial/ethnic disparities in suicide attempts, in conjunction with lower mental health care use among these groups, there is an urgent need to implement inclusive prevention and intervention strategies. These may include culturally and linguistically appropriate screening and assessments across both general and mental health care settings.
Appendix
Limitations
The study is based on 2015-19 data from the National Survey on Drug Use and Health (NSDUH), an annual behavioral health survey conducted by the U.S. Substance Abuse and Mental Health Services Administration that provides nationally representative data on substance use and disorders, mental health issues including suicide, and health care utilization related to these conditions. It is subject to the following limitations:
- All data is self-reported, so it is limited to the respondent’s memory and willingness to share. Although the survey uses interviewing techniques to enhance privacy and confidentiality, the questions cover sensitive behavioral health topics, which may result in under-reporting of mental health symptoms and substance use.
- The survey includes behavioral health variables (e.g., major depressive episodes, substance use disorders) that are based on validated screeners, but the responses may not always align with clinical diagnoses or alternate measures.
- The survey does not capture certain high-risk groups, including unhoused or institutionalized (e.g., incarcerated) people. In addition, it records sex only in the categories of males and females, precluding understanding of the relationship between other gender identities (e.g., transgender) and suicidal ideation, suicide attempts, and health care utilization. The results cannot be generalized to these groups.
- Suicide attempts can be impulsive and unplanned and may not always be preceded by ideation, but the survey asks about attempts only if people first affirm that they have thought about suicide. This precludes understanding of attempts for people who do not report seriously thinking about suicide.
- Although the survey includes a range of sociodemographic, behavioral, and related variables, other unmeasured social and structural factors, such as racism or environmental/life stressors, may still have an impact on ideation and attempts, which may confound the data.
- The survey asks respondents if they interacted with the health care system within a year of taking the survey, but it does not clarify whether that interaction preceded, followed, or was otherwise related to suicidal ideation or attempts. As a result, it is not possible to distinguish people who received care specifically for suicide risk.
- While the data is recent, longer-term trends are important to understand shifting risks, particularly related to COVID-19. However, NSDUH data after 2019 is not comparable to the data used in this study because the 2020 survey was disrupted during the pandemic and the 2021 survey added a new web-based interviewing technique.
Methodology
Sample
Data for this study was derived from the National Survey of Drug Use and Health (NSDUH) for 2015-19. The annual weighted responses of adults who were sampled through a multistage probability sampling frame were analyzed. The full sample included 214,505 adults.
Measures
Past-year suicidal ideation: Respondents were asked, “At any time in the past 12 months did you seriously think about trying to kill yourself?” A total of 13,195 adults reported past-year suicidal ideation.
Past-year suicide attempt: If a respondent answered yes to the question above, they were then asked, “At any time in the past 12 months did you try to kill yourself?” A total of 2,009 of the 13,195 who reported suicidal ideation also reported a suicide attempt in the past year.
Sociodemographic characteristics: Respondents reported certain sociodemographic information about themselves, including sex (males, females), age (18-25, 26-34, 35-49, 50-64, 65+), race/ethnicity (White, Black, Hispanic, Asian/Pacific Islander, Native American/Alaska Native, multiracial/other), education (less than high school, high school or equivalent, associate degree, some college, college degree), employment (full-time, part-time/other, unemployed), income (<$20,000, $20,000-$49,999, $50,000-$74,999, $75,000+), insurance (private, Medicare, Medicaid, military, none/other), marital status (single, married, divorced/separated/widowed), sexual orientation (heterosexual/straight, lesbian/gay, bisexual, unknown), and urbanicity (urban/rural). Data presented in Parts I, II, and IV is adjusted for sociodemographic characteristics.
Behavioral characteristics (no past-year substance use, past-year use without a disorder, or past-year substance use disorder): Data presented in Parts I, II, and IV of the interactive is adjusted for behavioral characteristics.
Clinical characteristics (health and mental health): Data presented in parts I, II, and IV of the interactive is adjusted for clinical characteristics.
Statistical analyses
Part I
To examine changes over time in suicidal ideation and attempts between groups, a series of separate logistic regressions was completed. Logistic regression aims to reveal associations between a set of characteristics and a binary outcome. In these models, the outcomes were Yes or No for suicidal ideation within the full sample, then Yes or No for suicide attempt within those who reported suicidal ideation. Each categorical characteristic listed above was included in the models as a variable or predictor of the binary outcome. For all categorical variables, a reference group (see glossary) was chosen. The reference group is generally the most common category or the category that makes interpretation easiest. Statistical interaction terms were included in these models for sex x year, age x year, and race x year in six separate models (three for suicidal ideation and three for suicide attempt). The models controlled for all other sociodemographic, substance use, and health variables. Only the results of significant interaction terms are shown in Part I.
Part II
To understand group differences within all categories, another series of logistic regression models predicting Yes or No for suicidal ideation within the full sample then predicting Yes or No for suicide attempt among those who reported suicidal ideation was performed. Each categorical characteristic listed above was again included in the models as a variable or predictor of the binary outcome with a reference group. In this analysis, for sociodemographic characteristics, generally the category with the most respondents was chosen as a reference group, except for age and urbanicity, for which the reference group was chosen to be the group at lowest suicide risk for ease of interpretability. For substance use and health variables, “No use” and better health outcomes were the reference groups, again for ease of interpretability. Because of the inclusion of all sociodemographic, substance use, and health characteristics in these analyses, results of the models are statistically controlling for all other characteristics. Results of the analysis are presented as predicted probabilities. Note that only comparisons between sociodemographic groups are reported in this brief. To see comparisons of substance use groups and health groups, see Table 2 in the manuscript linked below.
Part III
Prevalence of both suicidal ideation and suicide attempts was calculated and survey-weighted for each year of the 2015-19 dataset. Statistical tests determined whether ideation and attempt prevalence significantly changed from 2015 to 2019. These changes were tested over time only within each group (e.g., change over time for men, change over time for females). Group differences in prevalence trends of ideation and attempts were not compared (e.g., change over time for males was not compared with females) in these analyses. Note that only prevalence trends for sociodemographic groups are reported in this brief. To see prevalence trends for substance use groups and health groups, see Supplemental Tables S1 and S2 in the manuscript linked below.
Part IV
A final series of logistic regression models was conducted to understand the probability of health care utilization in various settings in the past year. For those with past-year suicidal ideation, one series of models predicted the probability of general health care usage in four different settings: any health care, inpatient, emergency department, outpatient. The next series of models predicted the probability of past-year mental health care usage in four different settings—any mental health care, inpatient, outpatient, and prescription services—for those with past-year suicidal ideation. Each model included all control variables of sociodemographic, substance use, and health characteristics. Given the potential to address suicide risk through clinical risk assessment, Part IV visualizes differences in probability of health care utilization of those with past-year suicidal ideation for sex, age, and race—characteristics for which data is regularly collected in clinical settings.
For more detailed information on the methodology and results, see the study in the journal Psychiatric Services.
Glossary
Adjusted estimate—Results for a desired outcome from a statistical model that controls for other variables that can impact the outcome. In this report, comparisons between groups (e.g., males or females) resulted in adjusted estimates when the statistical models controlled for other sociodemographic characteristics, substance use, and health variables.
Estimate—In this report, estimates are likelihood and refer to the predicted probability results of logistic regression. This term refers to the probability of a specific outcome (e.g., suicidal ideation or attempts) based on the variables of interest (e.g., sociodemographic characteristics) included in the chosen model.
Logistic regression—A statistical model that predicts the probability or odds of one event of a binary outcome occurring. In this case, “Yes” or “No” for suicidal ideation and suicide attempts and “Yes” or “No” for health care utilization in various settings were modeled with logistic regression.
Prevalence—Proportion of the full sample that reported suicidal ideation and proportion of those who reported suicidal ideation who also reported a suicide attempt.
Reference group—In a statistical model, when a variable of interest (e.g., sex, age, or race/ethnicity) comprises categories (e.g., males or females, or different racial/ethnic groups), one of the categories is chosen as the reference group with which all other categories are compared. When using reference groups, each category within a variable can be compared only with the chosen reference group. See methodology for explanation on how reference groups are chosen.
Statistically significant—In a statistical model, relationships between a characteristic (e.g., age or sex) and the outcome of interest (e.g., suicidal ideation or attempts) are statistically significant if the model determines that the relationship did not occur by chance. Here, consistent with statistical best practices, statistical significance was determined if the probability value (p-value) of the relationship was less than 0.05, determining that there is a less than 5% likelihood that a relationship between the characteristic and the outcome occurred because of chance.
Trend—A pattern over time. In this report, annual (yearly) prevalence trends from 2015 to 2019 and trends in likelihood of suicidal ideation and attempts from 2015 to 2019 were examined.
Unadjusted estimates—Results for a desired outcome from a statistical model that does not control for other variables that can impact the outcome. In this report, prevalence trends were controlled only for time (changes in prevalence from 2015 to 2019), not for sociodemographic, substance use, or health variables.